Tuesday Poster Session
Category: Biliary/Pancreas
P2860 - Septic Shock and Acute Kidney Injury Are Predictors of In-Hospital Mortality Among Prediabetic Pancreatic Cancer Patients: A Nationwide Inpatient Sample Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sheena Bhushan, MD
Northeast Georgia Medical Center
Atlanta, GA
Presenting Author(s)
Sheena Bhushan, MD1, Ange Ahoussougbemey, MD2, Shane Robinson, MS2, Riaz Mahmood, DO2
1Northeast Georgia Medical Center, Atlanta, GA; 2Northeast Georgia Medical Center, Gainesville, GA
Introduction: Pancreatic cancer and cardiovascular disease have shared risk factors, including obesity, smoking, and type 2 diabetes mellitus. Additionally, chemotherapeutic agents have been associated with acute coronary syndrome and implicated in other complications, including stroke, acute kidney injury, gastrointestinal bleeding, severe sepsis with shock, coagulopathy, and liver cirrhosis. This study aims to evaluate the outcomes of patients presenting with pancreatic cancer with prediabetes utilizing the National Inpatient Sample (NIS) database from 2016 to 2018.
Methods: A retrospective analysis of the NIS database from 2016 to 2018 was done to identify patients with a primary pancreatic cancer diagnosis using the International Classification of Diseases, 10th Edition codes. We compared the primary outcome of in-hospital mortality and the secondary outcomes of length of stay and total hospitalization cost. Multivariate logistic regression analysis was done to identify associations of in-hospital mortality.
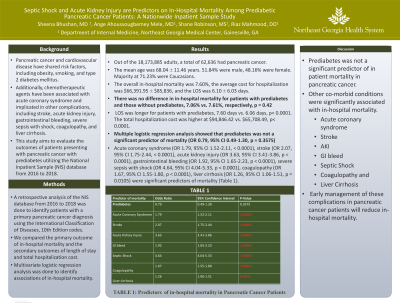
Results: From the 18,173,885 adults, a total of 62,636 had pancreatic cancer, with mean age 68.04 ± 11.46 years. 51.84% were male, and 71.23% were Caucasians. The overall in-hospital mortality was 7.60%, the average cost for hospitalization was $66,391.95 ± $85,836, and the LOS was 6.10 ± 6.03 days. There was no difference in in-hospital mortality for patients with prediabetes and those without prediabetes, 7.06% vs. 7.61%, respectively, p = 42.53. LOS was longer for patients with prediabetes, 7.60 days vs. 6.06 days, p< 0.0001. The total hospitalization cost was higher at $94,846.42 vs. $65,708.49, p< 0.0001. Multiple logistic regression analysis showed that prediabetes was not a significant predictor of mortality (OR 0.79, 95% CI 0.49-1.30, p = 0.3575); Acute coronary syndrome (OR 1.79, 95% CI 1.52-2.11, < 0.0001), stroke (OR 2.07, 95% CI 1.75-2.44, < 0.0001), acute kidney injury (OR 3.63, 95% CI 3.41-3.86, p < 0.0001), gastrointestinal bleeding (OR 1.92, 95% CI 1.65-2.23, p < 0.0001), severe sepsis with shock (OR 4.64, 95% CI 4.04-5.33, p < 0.0001), coagulopathy (OR 1.67, 95% CI 1.55-1.80, p < 0.0001), liver cirrhosis (OR 1.26, 95% CI 1.06-1.51, p = 0.0105) were significant predictors of mortality.
Discussion: Although prediabetes was not a significant predictor of mortality in pancreatic cancer, other co-morbid conditions, were significantly associated with in-hospital mortality. Early management of these complications in pancreatic cancer patients will reduce in-hospital mortality.
Disclosures:
Sheena Bhushan, MD1, Ange Ahoussougbemey, MD2, Shane Robinson, MS2, Riaz Mahmood, DO2. P2860 - Septic Shock and Acute Kidney Injury Are Predictors of In-Hospital Mortality Among Prediabetic Pancreatic Cancer Patients: A Nationwide Inpatient Sample Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Northeast Georgia Medical Center, Atlanta, GA; 2Northeast Georgia Medical Center, Gainesville, GA
Introduction: Pancreatic cancer and cardiovascular disease have shared risk factors, including obesity, smoking, and type 2 diabetes mellitus. Additionally, chemotherapeutic agents have been associated with acute coronary syndrome and implicated in other complications, including stroke, acute kidney injury, gastrointestinal bleeding, severe sepsis with shock, coagulopathy, and liver cirrhosis. This study aims to evaluate the outcomes of patients presenting with pancreatic cancer with prediabetes utilizing the National Inpatient Sample (NIS) database from 2016 to 2018.
Methods: A retrospective analysis of the NIS database from 2016 to 2018 was done to identify patients with a primary pancreatic cancer diagnosis using the International Classification of Diseases, 10th Edition codes. We compared the primary outcome of in-hospital mortality and the secondary outcomes of length of stay and total hospitalization cost. Multivariate logistic regression analysis was done to identify associations of in-hospital mortality.
Results: From the 18,173,885 adults, a total of 62,636 had pancreatic cancer, with mean age 68.04 ± 11.46 years. 51.84% were male, and 71.23% were Caucasians. The overall in-hospital mortality was 7.60%, the average cost for hospitalization was $66,391.95 ± $85,836, and the LOS was 6.10 ± 6.03 days. There was no difference in in-hospital mortality for patients with prediabetes and those without prediabetes, 7.06% vs. 7.61%, respectively, p = 42.53. LOS was longer for patients with prediabetes, 7.60 days vs. 6.06 days, p< 0.0001. The total hospitalization cost was higher at $94,846.42 vs. $65,708.49, p< 0.0001. Multiple logistic regression analysis showed that prediabetes was not a significant predictor of mortality (OR 0.79, 95% CI 0.49-1.30, p = 0.3575); Acute coronary syndrome (OR 1.79, 95% CI 1.52-2.11, < 0.0001), stroke (OR 2.07, 95% CI 1.75-2.44, < 0.0001), acute kidney injury (OR 3.63, 95% CI 3.41-3.86, p < 0.0001), gastrointestinal bleeding (OR 1.92, 95% CI 1.65-2.23, p < 0.0001), severe sepsis with shock (OR 4.64, 95% CI 4.04-5.33, p < 0.0001), coagulopathy (OR 1.67, 95% CI 1.55-1.80, p < 0.0001), liver cirrhosis (OR 1.26, 95% CI 1.06-1.51, p = 0.0105) were significant predictors of mortality.
Discussion: Although prediabetes was not a significant predictor of mortality in pancreatic cancer, other co-morbid conditions, were significantly associated with in-hospital mortality. Early management of these complications in pancreatic cancer patients will reduce in-hospital mortality.
Disclosures:
Sheena Bhushan indicated no relevant financial relationships.
Ange Ahoussougbemey indicated no relevant financial relationships.
Shane Robinson indicated no relevant financial relationships.
Riaz Mahmood indicated no relevant financial relationships.
Sheena Bhushan, MD1, Ange Ahoussougbemey, MD2, Shane Robinson, MS2, Riaz Mahmood, DO2. P2860 - Septic Shock and Acute Kidney Injury Are Predictors of In-Hospital Mortality Among Prediabetic Pancreatic Cancer Patients: A Nationwide Inpatient Sample Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
