Tuesday Poster Session
Category: Biliary/Pancreas
P2867 - Pancreatic Adenocarcinoma in a Regional Health Network: Predictors of Early Diagnosis and Survival
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Aurasch Moaven, MD
University of Vermont Medical Center
Burlington, VT
Presenting Author(s)
Aurasch Moaven, MD1, Jason Heffley, MD1, Edwin Goncharuk, DO2, Amanda Kennedy, PharmD1, Siddique T. Akram, MD1, Bradley Tompkins, MPH1, Richard Zubarik, MD1
1University of Vermont Medical Center, Burlington, VT; 2University of Vermont Medical Center, Williston, VT
Introduction: Early detection of pancreatic adenocarcinoma (PAC) has been associated with improved survival. Evaluation of barriers to early detection can identify ways to improve access to diagnosis and treatment. The aims of this study are to report a regional 5-year survival rate for PAC, to identify barriers to early diagnosis, and to determine predictors of survival.
Methods: This retrospective cohort study included patients with PAC from January 2011 to December 2021. The patients were identified from cancer registries of six hospitals comprising the University of Vermont Health Network (UVMHN). Patients with a pancreatic neoplasm other than PAC were excluded. The electronic health record was used to collect demographic data, baseline medical history, physician treatment team, diagnostic method, cancer location, stage at diagnosis, treatment type, and patient outcomes. Patients with stage 1 or 2 were considered resectable. Univariate and multivariate analyses were performed to evaluate for covariates associated with survival and early diagnosis. Patients who underwent surgery for curative intent were grouped by whether or not they had surgery at a very high-volume institution (defined as >90 cases/year).
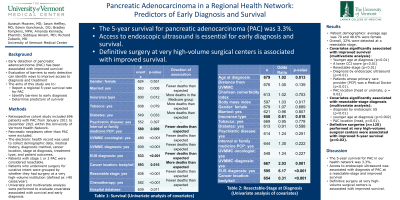
Results: There were 696 patients in the cohort. The average age was 70, and 48.6% were female. Overall, 32% were detected at a resectable stage. The 5-year survival rate was 3.3% (21/645). Variables significantly associated with improved survival include: younger age at diagnosis (p< 0.01), a lower Charlson Comorbidity Index score (p< 0.01), resectable-stage (p< 0.01), diagnosis by endoscopic ultrasound (p< 0.01), and diagnosis at the academic medical center (p< 0.01). Furthermore, patients whose primary care provider (PCP) was a Medical Doctor had improved survival (p< 0.01). Diabetes (p=0.03) and PAC location (body or tail, p=0.02) were associated with worse survival. Covariates significantly associated with resectable-stage diagnosis include diagnosis by endoscopic ultrasound (p< 0.01), diagnosis at the academic medical center (p< 0.01), and PAC location (head, p< 0.01). 125 patients underwent definitive surgery. Definitive surgeries performed at very high-volume surgical centers were associated with improved 5-year survival (p=0.02).
Discussion: The 5-year survival for PAC in our Health Network was 3.3%. Access to endoscopic ultrasound is essential for early diagnosis and survival. Definitive surgery at very high-volume surgical centers is associated with improved survival.
Disclosures:
Aurasch Moaven, MD1, Jason Heffley, MD1, Edwin Goncharuk, DO2, Amanda Kennedy, PharmD1, Siddique T. Akram, MD1, Bradley Tompkins, MPH1, Richard Zubarik, MD1. P2867 - Pancreatic Adenocarcinoma in a Regional Health Network: Predictors of Early Diagnosis and Survival, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Vermont Medical Center, Burlington, VT; 2University of Vermont Medical Center, Williston, VT
Introduction: Early detection of pancreatic adenocarcinoma (PAC) has been associated with improved survival. Evaluation of barriers to early detection can identify ways to improve access to diagnosis and treatment. The aims of this study are to report a regional 5-year survival rate for PAC, to identify barriers to early diagnosis, and to determine predictors of survival.
Methods: This retrospective cohort study included patients with PAC from January 2011 to December 2021. The patients were identified from cancer registries of six hospitals comprising the University of Vermont Health Network (UVMHN). Patients with a pancreatic neoplasm other than PAC were excluded. The electronic health record was used to collect demographic data, baseline medical history, physician treatment team, diagnostic method, cancer location, stage at diagnosis, treatment type, and patient outcomes. Patients with stage 1 or 2 were considered resectable. Univariate and multivariate analyses were performed to evaluate for covariates associated with survival and early diagnosis. Patients who underwent surgery for curative intent were grouped by whether or not they had surgery at a very high-volume institution (defined as >90 cases/year).
Results: There were 696 patients in the cohort. The average age was 70, and 48.6% were female. Overall, 32% were detected at a resectable stage. The 5-year survival rate was 3.3% (21/645). Variables significantly associated with improved survival include: younger age at diagnosis (p< 0.01), a lower Charlson Comorbidity Index score (p< 0.01), resectable-stage (p< 0.01), diagnosis by endoscopic ultrasound (p< 0.01), and diagnosis at the academic medical center (p< 0.01). Furthermore, patients whose primary care provider (PCP) was a Medical Doctor had improved survival (p< 0.01). Diabetes (p=0.03) and PAC location (body or tail, p=0.02) were associated with worse survival. Covariates significantly associated with resectable-stage diagnosis include diagnosis by endoscopic ultrasound (p< 0.01), diagnosis at the academic medical center (p< 0.01), and PAC location (head, p< 0.01). 125 patients underwent definitive surgery. Definitive surgeries performed at very high-volume surgical centers were associated with improved 5-year survival (p=0.02).
Discussion: The 5-year survival for PAC in our Health Network was 3.3%. Access to endoscopic ultrasound is essential for early diagnosis and survival. Definitive surgery at very high-volume surgical centers is associated with improved survival.
Disclosures:
Aurasch Moaven indicated no relevant financial relationships.
Jason Heffley indicated no relevant financial relationships.
Edwin Goncharuk indicated no relevant financial relationships.
Amanda Kennedy indicated no relevant financial relationships.
Siddique Akram indicated no relevant financial relationships.
Bradley Tompkins indicated no relevant financial relationships.
Richard Zubarik indicated no relevant financial relationships.
Aurasch Moaven, MD1, Jason Heffley, MD1, Edwin Goncharuk, DO2, Amanda Kennedy, PharmD1, Siddique T. Akram, MD1, Bradley Tompkins, MPH1, Richard Zubarik, MD1. P2867 - Pancreatic Adenocarcinoma in a Regional Health Network: Predictors of Early Diagnosis and Survival, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
