Tuesday Poster Session
Category: Biliary/Pancreas
P2884 - Outcomes of Patients Presenting With Acute Pancreatitis and Diabetic Ketoacidosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- DL
David Lehoang, MD, MBA
Keck School of Medicine of USC
Los Angeles, CA
Presenting Author(s)
David Lehoang, MD, MBA1, Thu Anne T. Mai, MD1, Matt Sumethasorn, MD1, Sarah Wang, MD, MPH1, Denis Nguyen, MD1, Paul Yoon, BA1, Sean Dewberry, MS1, Linda Huang, MD1, Mimi Xu, MD1, Jin Sun Kim, MD1, Alejandro Vazquez, BA1, Helen Lee, NP2, James Buxbaum, MD, MS1
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: There is limited understanding of the clinical course of concurrent diabetic ketoacidosis (DKA) and acute pancreatitis given its relative rarity. Preliminary work indicates that it poses a challenge with intravascular volume repletion strategies, glucose management, and initiation of a diet. We aim to explore the management and outcomes of concurrent DKA and acute pancreatitis.
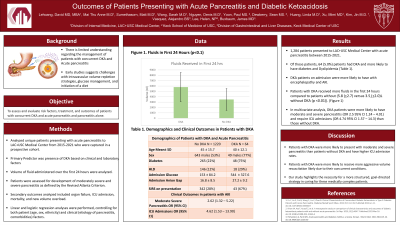
Methods: We analyzed all unique patients presenting with acute pancreatitis to Los Angeles General Medical Center captured in a prospective cohort. Our main predictor was the existence of DKA based on clinical and laboratory findings. Our primary outcome was development of moderate and severe pancreatitis according to the Revised Atlanta Criteria, and our secondary outcomes were development of SIRS, ICU admission, and mortality. Linear and logistic multivariate regression analyses were performed, controlling for both patient (such as age, sex, ethnicity) and clinical (eg etiology of pancreatitis, comorbidities) factors.
Results: Among 1,284 unique patients who presented to Los Angeles General Medical Center with acute pancreatitis between January 2015 and March 2021, 64 (5.0%) patients had concurrent DKA. Those with DKA were more likely to have comorbidities such as dyslipidemia (29% vs 12%, p < 0.01) and diabetes. They also were more likely to present with acute encephalopathy (23% vs 5%, p< 0.01) and acute renal failure. Patients with DKA received more fluids in the first 24 hours (5.8 (+2.7) versus 3.5 (+2.0)L without DKA (p < 0.01)). In multivariate analysis, DKA patients were more likely to have moderate and severe pancreatitis (OR 2.5 95% CI 1.24 – 4.01) and require ICU admissions (OR 4.74 95% CI 1.57 – 14.3) than those without DKA.
Discussion: Patients with DKA and acute pancreatitis are at higher risk for moderate and severe pancreatitis and necessity of ICU admission. While particularly aggressive volume resuscitation has been espoused for these patients, a more structured, goal-directed strategy could mitigate some of this observed morbidity.
Disclosures:
David Lehoang, MD, MBA1, Thu Anne T. Mai, MD1, Matt Sumethasorn, MD1, Sarah Wang, MD, MPH1, Denis Nguyen, MD1, Paul Yoon, BA1, Sean Dewberry, MS1, Linda Huang, MD1, Mimi Xu, MD1, Jin Sun Kim, MD1, Alejandro Vazquez, BA1, Helen Lee, NP2, James Buxbaum, MD, MS1. P2884 - Outcomes of Patients Presenting With Acute Pancreatitis and Diabetic Ketoacidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: There is limited understanding of the clinical course of concurrent diabetic ketoacidosis (DKA) and acute pancreatitis given its relative rarity. Preliminary work indicates that it poses a challenge with intravascular volume repletion strategies, glucose management, and initiation of a diet. We aim to explore the management and outcomes of concurrent DKA and acute pancreatitis.
Methods: We analyzed all unique patients presenting with acute pancreatitis to Los Angeles General Medical Center captured in a prospective cohort. Our main predictor was the existence of DKA based on clinical and laboratory findings. Our primary outcome was development of moderate and severe pancreatitis according to the Revised Atlanta Criteria, and our secondary outcomes were development of SIRS, ICU admission, and mortality. Linear and logistic multivariate regression analyses were performed, controlling for both patient (such as age, sex, ethnicity) and clinical (eg etiology of pancreatitis, comorbidities) factors.
Results: Among 1,284 unique patients who presented to Los Angeles General Medical Center with acute pancreatitis between January 2015 and March 2021, 64 (5.0%) patients had concurrent DKA. Those with DKA were more likely to have comorbidities such as dyslipidemia (29% vs 12%, p < 0.01) and diabetes. They also were more likely to present with acute encephalopathy (23% vs 5%, p< 0.01) and acute renal failure. Patients with DKA received more fluids in the first 24 hours (5.8 (+2.7) versus 3.5 (+2.0)L without DKA (p < 0.01)). In multivariate analysis, DKA patients were more likely to have moderate and severe pancreatitis (OR 2.5 95% CI 1.24 – 4.01) and require ICU admissions (OR 4.74 95% CI 1.57 – 14.3) than those without DKA.
Discussion: Patients with DKA and acute pancreatitis are at higher risk for moderate and severe pancreatitis and necessity of ICU admission. While particularly aggressive volume resuscitation has been espoused for these patients, a more structured, goal-directed strategy could mitigate some of this observed morbidity.
Disclosures:
David Lehoang indicated no relevant financial relationships.
Thu Anne Mai indicated no relevant financial relationships.
Matt Sumethasorn indicated no relevant financial relationships.
Sarah Wang indicated no relevant financial relationships.
Denis Nguyen indicated no relevant financial relationships.
Paul Yoon indicated no relevant financial relationships.
Sean Dewberry indicated no relevant financial relationships.
Linda Huang indicated no relevant financial relationships.
Mimi Xu indicated no relevant financial relationships.
Jin Sun Kim indicated no relevant financial relationships.
Alejandro Vazquez indicated no relevant financial relationships.
Helen Lee indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
David Lehoang, MD, MBA1, Thu Anne T. Mai, MD1, Matt Sumethasorn, MD1, Sarah Wang, MD, MPH1, Denis Nguyen, MD1, Paul Yoon, BA1, Sean Dewberry, MS1, Linda Huang, MD1, Mimi Xu, MD1, Jin Sun Kim, MD1, Alejandro Vazquez, BA1, Helen Lee, NP2, James Buxbaum, MD, MS1. P2884 - Outcomes of Patients Presenting With Acute Pancreatitis and Diabetic Ketoacidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
