Tuesday Poster Session
Category: Biliary/Pancreas
P2885 - Management of Surgically High-Risk Patients With Acute Cholecystitis: A Comparative Retrospective Study of Percutaneous Cholecystostomy vs Endoscopic Retrograde Cholangiopancreatography Gallbladder Drainage
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- ME
Mohammed El-Dallal, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, West Virginia
Presenting Author(s)
Mohammed El-Dallal, MD1, Abdelwahap Elghezewi, MD2, Onyinye Ugonabo, MD1, Mohamed Hammad, MD2, M'hamed Turki, MD1, Tewodros T. Ayele, MD1, Hafiz Zarsham Ali Ikram, MD3, Bezaye Milkias, MD1, Omar Al Metwali, MD1, Mujtaba Mohamed, MBBS4, Adnan Khan, MD1, Ahmed Sherif, MD2, Wesam Frandah, MD1
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University, Huntington, WV; 3Marshall University School of Medicine, Huntington, WV; 4Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Gallbladder drainage is essential for high-risk patients with acute cholecystitis (AC) who cannot undergo surgery. Percutaneous cholecystostomy (PC) and endoscopic retrograde cholangiopancreatography (ERCP) are commonly used for biliary drainage. This study compares the effectiveness and outcomes of PC and ERCP in patients with AC who are ineligible for surgery.
Methods: Data were acquired from Marshall University hospitals, St Mary Medical Center and Cabell Huntington Hospital, Huntington, WV, from January 2019 to December 2022. AC patients deemed ineligible for cholecystectomy were classified into PC and ERCP groups. Chart reviews captured vital signs, lab results, comorbidities, surgical history, American Society of Anesthesiologists classification, and drainage procedure details. Outcomes assessed included technical and clinical successes, hospital mortality, 30-day mortality, unplanned procedures and hospital readmission within 30 days, post procedure complications (including luminal perforation, bile leak, stent/tube dislodgment, pancreatitis, bleeding, or infection), and length of stay (LOS). Chi-square test was used to examine categorical variables and t-test for continuous variables. Logistic regression model was built to adjust the differences between the groups.
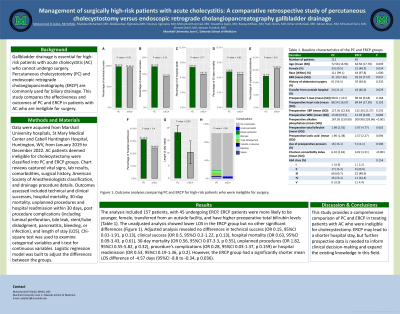
Results: The analysis included 157 patients, with 45 undergoing ERCP. ERCP patients were more likely to be younger, female, transferred from an outside facility, and have higher preoperative total bilirubin levels (Table 1). The unadjusted analysis showed lower LOS in the ERCP group but no other significant differences (Figure 1). Adjusted analysis revealed no differences in technical success (OR 0.15, 95%CI 0.01-1.91, p 0.13), clinical success (OR 0.5, 95%CI 0.2-1.22, p 0.13), hospital mortality (OR 0.63, 95%CI 0.09-3.43, p 0.61), 30-day mortality (OR 0.56, 95%CI 0.07-3.3, p 0.55), unplanned procedures (OR 1.82, 95%CI 0.55-5.82, p 0.32), procedure’s complications (OR 0.28, 95%CI 0.03-1.37, p 0.159) or hospital readmission (OR 0.53, 95%CI 0.19-1.36, p 0.2). However, the ERCP group had a significantly shorter mean LOS difference of -4.57 days (95%CI -8.8 to -0.34, p 0.036).
Discussion: This study provides a comprehensive comparison of PC and ERCP in treating patients with AC who were ineligible for cholecystectomy. ERCP may lead to a shorter hospital stay, but further prospective data is needed to inform clinical decision-making and expand the existing knowledge in this field.

Disclosures:
Mohammed El-Dallal, MD1, Abdelwahap Elghezewi, MD2, Onyinye Ugonabo, MD1, Mohamed Hammad, MD2, M'hamed Turki, MD1, Tewodros T. Ayele, MD1, Hafiz Zarsham Ali Ikram, MD3, Bezaye Milkias, MD1, Omar Al Metwali, MD1, Mujtaba Mohamed, MBBS4, Adnan Khan, MD1, Ahmed Sherif, MD2, Wesam Frandah, MD1. P2885 - Management of Surgically High-Risk Patients With Acute Cholecystitis: A Comparative Retrospective Study of Percutaneous Cholecystostomy vs Endoscopic Retrograde Cholangiopancreatography Gallbladder Drainage, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University, Huntington, WV; 3Marshall University School of Medicine, Huntington, WV; 4Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Gallbladder drainage is essential for high-risk patients with acute cholecystitis (AC) who cannot undergo surgery. Percutaneous cholecystostomy (PC) and endoscopic retrograde cholangiopancreatography (ERCP) are commonly used for biliary drainage. This study compares the effectiveness and outcomes of PC and ERCP in patients with AC who are ineligible for surgery.
Methods: Data were acquired from Marshall University hospitals, St Mary Medical Center and Cabell Huntington Hospital, Huntington, WV, from January 2019 to December 2022. AC patients deemed ineligible for cholecystectomy were classified into PC and ERCP groups. Chart reviews captured vital signs, lab results, comorbidities, surgical history, American Society of Anesthesiologists classification, and drainage procedure details. Outcomes assessed included technical and clinical successes, hospital mortality, 30-day mortality, unplanned procedures and hospital readmission within 30 days, post procedure complications (including luminal perforation, bile leak, stent/tube dislodgment, pancreatitis, bleeding, or infection), and length of stay (LOS). Chi-square test was used to examine categorical variables and t-test for continuous variables. Logistic regression model was built to adjust the differences between the groups.
Results: The analysis included 157 patients, with 45 undergoing ERCP. ERCP patients were more likely to be younger, female, transferred from an outside facility, and have higher preoperative total bilirubin levels (Table 1). The unadjusted analysis showed lower LOS in the ERCP group but no other significant differences (Figure 1). Adjusted analysis revealed no differences in technical success (OR 0.15, 95%CI 0.01-1.91, p 0.13), clinical success (OR 0.5, 95%CI 0.2-1.22, p 0.13), hospital mortality (OR 0.63, 95%CI 0.09-3.43, p 0.61), 30-day mortality (OR 0.56, 95%CI 0.07-3.3, p 0.55), unplanned procedures (OR 1.82, 95%CI 0.55-5.82, p 0.32), procedure’s complications (OR 0.28, 95%CI 0.03-1.37, p 0.159) or hospital readmission (OR 0.53, 95%CI 0.19-1.36, p 0.2). However, the ERCP group had a significantly shorter mean LOS difference of -4.57 days (95%CI -8.8 to -0.34, p 0.036).
Discussion: This study provides a comprehensive comparison of PC and ERCP in treating patients with AC who were ineligible for cholecystectomy. ERCP may lead to a shorter hospital stay, but further prospective data is needed to inform clinical decision-making and expand the existing knowledge in this field.

Figure: Figure 1. Unadjusted outcome analysis comparing percutaneous cholecystostomy (PC) and endoscopic retrograde cholangiopancreatography (ERCP) for high-risk patients who were ineligible for surgery.
Disclosures:
Mohammed El-Dallal indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Onyinye Ugonabo indicated no relevant financial relationships.
Mohamed Hammad indicated no relevant financial relationships.
M'hamed Turki indicated no relevant financial relationships.
Tewodros Ayele indicated no relevant financial relationships.
Hafiz Zarsham Ali Ikram indicated no relevant financial relationships.
Bezaye Milkias indicated no relevant financial relationships.
Omar Al Metwali indicated no relevant financial relationships.
Mujtaba Mohamed indicated no relevant financial relationships.
Adnan Khan indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Endo gastric solutions – Consultant. Olympus Medical – Consultant.
Mohammed El-Dallal, MD1, Abdelwahap Elghezewi, MD2, Onyinye Ugonabo, MD1, Mohamed Hammad, MD2, M'hamed Turki, MD1, Tewodros T. Ayele, MD1, Hafiz Zarsham Ali Ikram, MD3, Bezaye Milkias, MD1, Omar Al Metwali, MD1, Mujtaba Mohamed, MBBS4, Adnan Khan, MD1, Ahmed Sherif, MD2, Wesam Frandah, MD1. P2885 - Management of Surgically High-Risk Patients With Acute Cholecystitis: A Comparative Retrospective Study of Percutaneous Cholecystostomy vs Endoscopic Retrograde Cholangiopancreatography Gallbladder Drainage, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
