Tuesday Poster Session
Category: Biliary/Pancreas
P2916 - A Case Report of Poor-Prognostic Pancreatic Neuroendocrine Tumor
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- NS
Nishith Sripathi, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Nishith Sripathi, MD, Tushita Verma, DO, MPH, Niloy Ghosh, MD, Farzana Harji, MD
University of New Mexico Health Sciences Center, Albuquerque, NM
Introduction: Pancreatic neuroendocrine tumors (PNETs) account for approximately 1-2% of all pancreatic tumors and can be functional or more commonly non-functional (approximately 75-90%). Mortality rates increase with metastasis of the disease and early detection is crucial. However, detection is often difficult and occurs later in disease course. This case represents late detection of a rapidly progressing rare PNET.
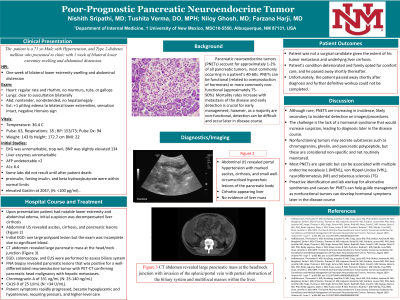
Case Description/Methods: A 71-year-old male with Type 2 DM presented with worsening bilateral lower extremity edema and abdominal distension. Admission labs included a Chromogranin A of 331 ng/mL and CA19-9 of 25 U/mL. Abdominal US revealed portal hypertension with marked ascites, cirrhosis, and small well-circumscribed hypoechoic lesions of the pancreatic body. CT abdomen revealed a large pancreatic mass at the head/neck junction with invasion of the splenic/portal vein, partial obstruction of the biliary system, and multifocal masses within the liver. FNA biopsy of pancreatic lesions was positive for a well-differentiated neuroendocrine tumor with PET-CT confirming pancreatic head malignancy with hepatic metastases. The patient was not a surgical candidate given the extent of his tumor metastasis and underlying liver cirrhosis. His condition deteriorated and family opted for comfort care, and he passed away shortly thereafter. Posthumous labs showed proinsulin, fasting insulin, and beta hydroxybutyrate within normal limits and an elevated Gastrin of 2047.
Discussion: Although rare, PNETs are increasing in incidence likely secondary to detection on images/procedures for alternate concerns. Non-functional PNETs are particularly hard to diagnose given the lack of a hormonal syndrome that would increase suspicion, leading to diagnosis later in disease course. Nonfunctioning tumors may secrete substances such as chromogranin, ghrelin, and pancreatic polypeptide, but these are considered non-specific and not routinely monitored.
Most PNETs are sporadic but can be associated with MEN1, VHL, NF, and tuberous sclerosis. If associated with an underlying syndrome, treatment and prognostics differ compared to sporadic mutations. Surgical resection is generally preferred but is not always an option. Unfortunately, our patient passed away shortly after diagnosis and further definitive workup could not be completed. Proactive identification and lab workup for alternative etiologies for PNETs can help guide management as nonfunctional tumors can develop hormonal symptoms later in their disease course.

Disclosures:
Nishith Sripathi, MD, Tushita Verma, DO, MPH, Niloy Ghosh, MD, Farzana Harji, MD. P2916 - A Case Report of Poor-Prognostic Pancreatic Neuroendocrine Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of New Mexico Health Sciences Center, Albuquerque, NM
Introduction: Pancreatic neuroendocrine tumors (PNETs) account for approximately 1-2% of all pancreatic tumors and can be functional or more commonly non-functional (approximately 75-90%). Mortality rates increase with metastasis of the disease and early detection is crucial. However, detection is often difficult and occurs later in disease course. This case represents late detection of a rapidly progressing rare PNET.
Case Description/Methods: A 71-year-old male with Type 2 DM presented with worsening bilateral lower extremity edema and abdominal distension. Admission labs included a Chromogranin A of 331 ng/mL and CA19-9 of 25 U/mL. Abdominal US revealed portal hypertension with marked ascites, cirrhosis, and small well-circumscribed hypoechoic lesions of the pancreatic body. CT abdomen revealed a large pancreatic mass at the head/neck junction with invasion of the splenic/portal vein, partial obstruction of the biliary system, and multifocal masses within the liver. FNA biopsy of pancreatic lesions was positive for a well-differentiated neuroendocrine tumor with PET-CT confirming pancreatic head malignancy with hepatic metastases. The patient was not a surgical candidate given the extent of his tumor metastasis and underlying liver cirrhosis. His condition deteriorated and family opted for comfort care, and he passed away shortly thereafter. Posthumous labs showed proinsulin, fasting insulin, and beta hydroxybutyrate within normal limits and an elevated Gastrin of 2047.
Discussion: Although rare, PNETs are increasing in incidence likely secondary to detection on images/procedures for alternate concerns. Non-functional PNETs are particularly hard to diagnose given the lack of a hormonal syndrome that would increase suspicion, leading to diagnosis later in disease course. Nonfunctioning tumors may secrete substances such as chromogranin, ghrelin, and pancreatic polypeptide, but these are considered non-specific and not routinely monitored.
Most PNETs are sporadic but can be associated with MEN1, VHL, NF, and tuberous sclerosis. If associated with an underlying syndrome, treatment and prognostics differ compared to sporadic mutations. Surgical resection is generally preferred but is not always an option. Unfortunately, our patient passed away shortly after diagnosis and further definitive workup could not be completed. Proactive identification and lab workup for alternative etiologies for PNETs can help guide management as nonfunctional tumors can develop hormonal symptoms later in their disease course.

Figure: Large pancreatic mass at the head/neck junction with invasion of the splenic/portal vein with partial obstruction of the biliary system and multifocal masses within the liver
Disclosures:
Nishith Sripathi indicated no relevant financial relationships.
Tushita Verma indicated no relevant financial relationships.
Niloy Ghosh indicated no relevant financial relationships.
Farzana Harji indicated no relevant financial relationships.
Nishith Sripathi, MD, Tushita Verma, DO, MPH, Niloy Ghosh, MD, Farzana Harji, MD. P2916 - A Case Report of Poor-Prognostic Pancreatic Neuroendocrine Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
