Tuesday Poster Session
Category: Liver
P3919 - Multiorgan Failure Following Acute Hepatitis E Infection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sharon Slomovich, MD
Mount Sinai South Nassau
Oceanside, NY
Presenting Author(s)
Sharon Slomovich, MD1, Visala Natarajan, MBA1, Gal Rubinstein, MD2, Pavel Gozenput, MD1, Benhoor Shamian, MD1
1Mount Sinai South Nassau, Oceanside, NY; 2Jacobi Medical Center, Bronx, NY
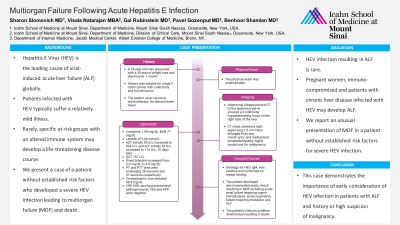
Introduction: Hepatitis E Virus (HEV) is the leading cause of viral-induced acute liver failure (ALF) globally. Patients infected with HEV typically suffer a relatively mild illness. Rarely, specific at-risk groups with an altered immune system may develop a life-threatening disease course. We present a case of a patient without established risk factors who developed a severe HEV infection leading to multiorgan failure (MOF) and death.
Case Description/Methods: A 79-year-old man presented with a 30-pound weight loss and diarrhea for 1 month. Medical history was notable for stage II colon cancer with colectomy and full remission and urothelial papillary carcinoma status post tubal resection. The patient never received chemotherapy or radiation. He denied any recent travel.
The physical exam was unremarkable. Laboratory data revealed a BUN of 77 mg/dL, creatinine of 1.59 mg/dL and a lactate of 5.66 mmol/L. AST initially 95 U/L increased to 934 U/L and ALT initially 53 U/L, increased to 114 U/L, 10 days later. GGT was 157 U/L and direct bilirubin increased from 2.0 mg/dL to 4.0 md/dL. PT and PTT time were prolonged, 28 seconds and 41 seconds respectively. Ceruloplasmin was elevated 38.5 mg/dL. CRP, ESR, stool gastrointestinal pathogen panel, CEA and AFP were negative. Abdominal ultrasound and CT of the abdomen and pelvis were consistent with a 2-millimeter hypoattenuating focus on the right lobe of the liver.
The patient was treated empirically with broad-spectrum antibiotics. Further workup including blood and urine cultures, antibodies for hepatitis A, B and C, Epstein-Barr virus, and cytomegalovirus were unremarkable. Serology for HEV, IgM, was positive and confirmed on repeat testing.
The patient developed decompensated septic shock resulting in MOF including acute renal failure requiring urgent hemodialysis, acute respiratory failure requiring intubation and ALF. CT chest demonstrated a right upper lung 2.3-cm mass, enlarged from one month prior, and mediastinal lymphadenopathy, highly suspicious for malignancy. The patient’s clinical condition deteriorated resulting in death.
Discussion: HEV infection resulting in ALF is rare. Pregnant women, immunocompromised individuals and patients with chronic liver disease infected with HEV may develop ALF. We report an unusual presentation of MOF in a patient without established risk factors for severe HEV infection. This case demonstrates the importance of early consideration of HEV infection in patients with ALF and history or high suspicion of malignancy.
Disclosures:
Sharon Slomovich, MD1, Visala Natarajan, MBA1, Gal Rubinstein, MD2, Pavel Gozenput, MD1, Benhoor Shamian, MD1. P3919 - Multiorgan Failure Following Acute Hepatitis E Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai South Nassau, Oceanside, NY; 2Jacobi Medical Center, Bronx, NY
Introduction: Hepatitis E Virus (HEV) is the leading cause of viral-induced acute liver failure (ALF) globally. Patients infected with HEV typically suffer a relatively mild illness. Rarely, specific at-risk groups with an altered immune system may develop a life-threatening disease course. We present a case of a patient without established risk factors who developed a severe HEV infection leading to multiorgan failure (MOF) and death.
Case Description/Methods: A 79-year-old man presented with a 30-pound weight loss and diarrhea for 1 month. Medical history was notable for stage II colon cancer with colectomy and full remission and urothelial papillary carcinoma status post tubal resection. The patient never received chemotherapy or radiation. He denied any recent travel.
The physical exam was unremarkable. Laboratory data revealed a BUN of 77 mg/dL, creatinine of 1.59 mg/dL and a lactate of 5.66 mmol/L. AST initially 95 U/L increased to 934 U/L and ALT initially 53 U/L, increased to 114 U/L, 10 days later. GGT was 157 U/L and direct bilirubin increased from 2.0 mg/dL to 4.0 md/dL. PT and PTT time were prolonged, 28 seconds and 41 seconds respectively. Ceruloplasmin was elevated 38.5 mg/dL. CRP, ESR, stool gastrointestinal pathogen panel, CEA and AFP were negative. Abdominal ultrasound and CT of the abdomen and pelvis were consistent with a 2-millimeter hypoattenuating focus on the right lobe of the liver.
The patient was treated empirically with broad-spectrum antibiotics. Further workup including blood and urine cultures, antibodies for hepatitis A, B and C, Epstein-Barr virus, and cytomegalovirus were unremarkable. Serology for HEV, IgM, was positive and confirmed on repeat testing.
The patient developed decompensated septic shock resulting in MOF including acute renal failure requiring urgent hemodialysis, acute respiratory failure requiring intubation and ALF. CT chest demonstrated a right upper lung 2.3-cm mass, enlarged from one month prior, and mediastinal lymphadenopathy, highly suspicious for malignancy. The patient’s clinical condition deteriorated resulting in death.
Discussion: HEV infection resulting in ALF is rare. Pregnant women, immunocompromised individuals and patients with chronic liver disease infected with HEV may develop ALF. We report an unusual presentation of MOF in a patient without established risk factors for severe HEV infection. This case demonstrates the importance of early consideration of HEV infection in patients with ALF and history or high suspicion of malignancy.
Disclosures:
Sharon Slomovich indicated no relevant financial relationships.
Visala Natarajan indicated no relevant financial relationships.
Gal Rubinstein indicated no relevant financial relationships.
Pavel Gozenput indicated no relevant financial relationships.
Benhoor Shamian indicated no relevant financial relationships.
Sharon Slomovich, MD1, Visala Natarajan, MBA1, Gal Rubinstein, MD2, Pavel Gozenput, MD1, Benhoor Shamian, MD1. P3919 - Multiorgan Failure Following Acute Hepatitis E Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
