Tuesday Poster Session
Category: Liver
P3927 - Mixed Liver Injury, Splenic Infarcts and Terminal Ileitis, a Rare Clinical Manifestation of Acute Epstein Barr Virus Infection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- JV
Jeremy Van, DO
University of Chicago/Northshore University
Evanston, IL
Presenting Author(s)
Jeremy Van, DO1, Ansa Mehreen, MD2, Omar Khan, MD3
1University of Chicago/Northshore University, Evanston, IL; 2University of Chicago/Northshore, Chicago, IL; 3North Shore University Health System, Evanston, IL
Introduction: Epstein Barr Virus (EBV) is a herpesvirus commonly disseminated via oropharyngeal/nasopharyngeal secretions. It classically presents as fever, pharyngitis, lymphadenopathy (LAD), and fatigue. Rarely, patients (pts) develop cholestatic/hepatocellular (mixed) liver injury, splenic infarcts (SI) and terminal ileitis (TI). We describe such a case here.
Case Description/Methods: 26 year old female with no past medical history presented to the hospital with (w/) one week history of fever, nausea, bilateral upper quadrant abdominal pain, and diarrhea. She was not on any medications or herbal supplements. She had tenderness to palpation in the bilateral upper quadrants; no evidence of pharyngitis or LAD on exam. WBC 8.0 K/uL, Hgb 15.0 g/dL, platelets 202 K/uL, blood smear w/ atypical lymphocytes, albumin 3.3 g/dL, INR 1.1, total bilirubin (bili) 3.5 mg/dL, direct bili 2.7 mg/dL, ALP 234 U/L, AST 187 U/L, ALT 300 U/L. LFT’s were normal one month prior. Hep A, B, and C serologies were unremarkable. Monospot test was negative (neg), Tylenol level and urine drug screen were undetectable. Viral respiratory panel was neg. Infectious stool studies were neg. CT abdomen and pelvis (A/P) with IV contrast demonstrated SI and TI. Vascular duplex A/P showed patent hepatic and portal veins. Hypercoagulability workup was neg. ANA, ASMA, and ANCA were neg. TB QuantiFERON and HIV antigen/antibody were neg. MRA chest/A/P had no additional vascular abnormality. TEE had no valvular abnormality. CMV IgM/IgG was neg. EBV Viral Capsid Antigen (VCA) IgM was positive and EBV VCA IgG and Nuclear antigen IgG were neg. On liver biopsy, in-situ hybridization study for EBV encoded RNA demonstrated EBV positive lymphocytes. Her symptoms and liver enzymes improved with conservative management and was discharged w/ close outpatient follow up.
Discussion: This is the first case to our knowledge in the literature of an immunocompetent pt w/ acute EBV induced mixed liver injury, SI and TI. 80% of EBV pts have hepatocellular liver injury with < 5 fold increase in AST and ALT. Only 5% of pts will have hyperbilirubinemia either 2/2 hemolysis or intrahepatic cholestasis. SI are rare with unclear pathogenesis in this setting. Several proposed mechanisms include decreased arterial blood supply, transient hypercoagulable state and increased level of circulating immune complexes. EBV induced TI is typically described in immunocompromised pts or pts w/ IBD. The gold standard of EBV treatment is supportive care which was effective for this pt.

Disclosures:
Jeremy Van, DO1, Ansa Mehreen, MD2, Omar Khan, MD3. P3927 - Mixed Liver Injury, Splenic Infarcts and Terminal Ileitis, a Rare Clinical Manifestation of Acute Epstein Barr Virus Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Chicago/Northshore University, Evanston, IL; 2University of Chicago/Northshore, Chicago, IL; 3North Shore University Health System, Evanston, IL
Introduction: Epstein Barr Virus (EBV) is a herpesvirus commonly disseminated via oropharyngeal/nasopharyngeal secretions. It classically presents as fever, pharyngitis, lymphadenopathy (LAD), and fatigue. Rarely, patients (pts) develop cholestatic/hepatocellular (mixed) liver injury, splenic infarcts (SI) and terminal ileitis (TI). We describe such a case here.
Case Description/Methods: 26 year old female with no past medical history presented to the hospital with (w/) one week history of fever, nausea, bilateral upper quadrant abdominal pain, and diarrhea. She was not on any medications or herbal supplements. She had tenderness to palpation in the bilateral upper quadrants; no evidence of pharyngitis or LAD on exam. WBC 8.0 K/uL, Hgb 15.0 g/dL, platelets 202 K/uL, blood smear w/ atypical lymphocytes, albumin 3.3 g/dL, INR 1.1, total bilirubin (bili) 3.5 mg/dL, direct bili 2.7 mg/dL, ALP 234 U/L, AST 187 U/L, ALT 300 U/L. LFT’s were normal one month prior. Hep A, B, and C serologies were unremarkable. Monospot test was negative (neg), Tylenol level and urine drug screen were undetectable. Viral respiratory panel was neg. Infectious stool studies were neg. CT abdomen and pelvis (A/P) with IV contrast demonstrated SI and TI. Vascular duplex A/P showed patent hepatic and portal veins. Hypercoagulability workup was neg. ANA, ASMA, and ANCA were neg. TB QuantiFERON and HIV antigen/antibody were neg. MRA chest/A/P had no additional vascular abnormality. TEE had no valvular abnormality. CMV IgM/IgG was neg. EBV Viral Capsid Antigen (VCA) IgM was positive and EBV VCA IgG and Nuclear antigen IgG were neg. On liver biopsy, in-situ hybridization study for EBV encoded RNA demonstrated EBV positive lymphocytes. Her symptoms and liver enzymes improved with conservative management and was discharged w/ close outpatient follow up.
Discussion: This is the first case to our knowledge in the literature of an immunocompetent pt w/ acute EBV induced mixed liver injury, SI and TI. 80% of EBV pts have hepatocellular liver injury with < 5 fold increase in AST and ALT. Only 5% of pts will have hyperbilirubinemia either 2/2 hemolysis or intrahepatic cholestasis. SI are rare with unclear pathogenesis in this setting. Several proposed mechanisms include decreased arterial blood supply, transient hypercoagulable state and increased level of circulating immune complexes. EBV induced TI is typically described in immunocompromised pts or pts w/ IBD. The gold standard of EBV treatment is supportive care which was effective for this pt.

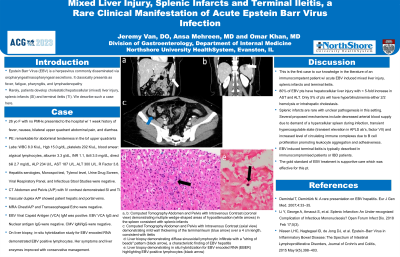
Figure: Figure 1 Image panel
a, b: Computed Tomography Abdomen and Pelvis with Intravenous Contrast (coronal view) demonstrating multiple wedge-shaped areas of hypoattenuation (white arrows) in the spleen consistent with splenic infarcts
c: Computed Tomography Abdomen and Pelvis with Intravenous Contrast (axial view) demonstrating wall thickening of the terminal ileum (blue arrow) over a 4 cm length, consistent with ileitis
d: Liver biopsy demonstrating diffuse sinusoidal lymphocytic infiltrate with a "string of beads" pattern (black arrow), a characteristic finding of EBV hepatitis
e: Liver biopsy demonstrating in situ hybridization for EBV encoded RNA (EBER) highlighting EBV-positive lymphocytes (black arrow)
a, b: Computed Tomography Abdomen and Pelvis with Intravenous Contrast (coronal view) demonstrating multiple wedge-shaped areas of hypoattenuation (white arrows) in the spleen consistent with splenic infarcts
c: Computed Tomography Abdomen and Pelvis with Intravenous Contrast (axial view) demonstrating wall thickening of the terminal ileum (blue arrow) over a 4 cm length, consistent with ileitis
d: Liver biopsy demonstrating diffuse sinusoidal lymphocytic infiltrate with a "string of beads" pattern (black arrow), a characteristic finding of EBV hepatitis
e: Liver biopsy demonstrating in situ hybridization for EBV encoded RNA (EBER) highlighting EBV-positive lymphocytes (black arrow)
Disclosures:
Jeremy Van indicated no relevant financial relationships.
Ansa Mehreen indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Jeremy Van, DO1, Ansa Mehreen, MD2, Omar Khan, MD3. P3927 - Mixed Liver Injury, Splenic Infarcts and Terminal Ileitis, a Rare Clinical Manifestation of Acute Epstein Barr Virus Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
