Tuesday Poster Session
Category: Liver
P3960 - The Cost of Curing Colon Cancer: Oxaliplatin-Induced NCPH-Related Colonic Bleeding
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PR
Pavithra Ramakrishnan, MS, MD
University of MInnesota
Minneapolis, MN
Presenting Author(s)
Pavithra Ramakrishnan, MS, MD1, Bryant Megna, MD2, Kawthar Mohamed, MD2, Oyedele Adeyi, MD3, Julie Thompson, MD2
1University of MInnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota Medical School, Minneapolis, MN
Introduction: Oxaliplatin is one of the main chemotherapeutic agents used as neoadjuvant or adjuvant treatment of metastatic colon cancer. A rarely reported side effect of this medication is hepatic sinusoidal/capillary epithelial damage leading to congestion and development of non-cirrhotic portal hypertension (NCPH). Herein we report a rare presentation of NCPH a decade after treatment with oxaliplatin for colon cancer, with recalcitrant bleeding at the coloanal anastomotic site.
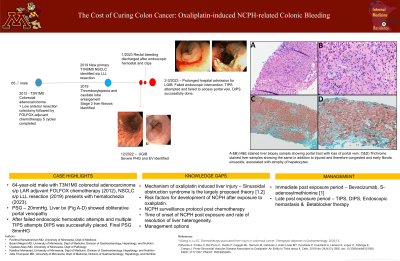
Case Description/Methods: A 64-year-old male with history of T3N1b colorectal adenocarcinoma was treated with low anterior resection with colostomy and Hartman pouch followed by adjuvant chemotherapy with FOLFOX and radiation therapy and by eventual colostomy reversal. Nearly a decade later, he presented with hematochezia which was found on colonoscopy to be originating at the coloanal anastomotic site. Severe portal hypertensive gastropathy and esophageal varices were identified on upper endoscopy. Bleeding was initially controlled with localized epinephrine injection, cautery and hemoclips (Figure 1a, 1b). MR elastography showed no evidence of cirrhosis. His hepatic vein portal venous gradient pressure was 4 mmHg and portosystemic gradient (PSG) was 20 mmHg, Liver biopsy showed obliterative portal venopathy without liver nodularity or fibrosis (Figure 1c-f). The diagnosis of oxaliplatin induced portosinusoidal vascular disease was made. Large volume rectal bleeding reoccurred on four instances in the following weeks, managed by cautery, hemoclips, and hemostatic spray, all to no avail. Non-occlusive SMV thrombus was also newly discovered on CT angiography. To control bleeding via reducing pressure in the portal system, transjugular intrahepatic portosystemic shunt placement was trialed but unsuccessful due to difficulties with accessing the portal vasculature. Subsequently, direct intrahepatic portocaval shunt was placed with a final PSG of 8mmHg and bleeding was controlled.
Discussion: Clinical presentation of NCPH has been reported to occur within a year of oxaliplatin exposure characterized by variceal bleeding, splenomegaly, or ascites with several underlying mechanisms proposed. Management of this condition follows the same guidelines as management of cirrhotic portal hypertension and cessation of oxaliplatin therapy. This case highlights the importance of vigilance for long-term complications in colon cancer patients treated with this agent.

Disclosures:
Pavithra Ramakrishnan, MS, MD1, Bryant Megna, MD2, Kawthar Mohamed, MD2, Oyedele Adeyi, MD3, Julie Thompson, MD2. P3960 - The Cost of Curing Colon Cancer: Oxaliplatin-Induced NCPH-Related Colonic Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of MInnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota Medical School, Minneapolis, MN
Introduction: Oxaliplatin is one of the main chemotherapeutic agents used as neoadjuvant or adjuvant treatment of metastatic colon cancer. A rarely reported side effect of this medication is hepatic sinusoidal/capillary epithelial damage leading to congestion and development of non-cirrhotic portal hypertension (NCPH). Herein we report a rare presentation of NCPH a decade after treatment with oxaliplatin for colon cancer, with recalcitrant bleeding at the coloanal anastomotic site.
Case Description/Methods: A 64-year-old male with history of T3N1b colorectal adenocarcinoma was treated with low anterior resection with colostomy and Hartman pouch followed by adjuvant chemotherapy with FOLFOX and radiation therapy and by eventual colostomy reversal. Nearly a decade later, he presented with hematochezia which was found on colonoscopy to be originating at the coloanal anastomotic site. Severe portal hypertensive gastropathy and esophageal varices were identified on upper endoscopy. Bleeding was initially controlled with localized epinephrine injection, cautery and hemoclips (Figure 1a, 1b). MR elastography showed no evidence of cirrhosis. His hepatic vein portal venous gradient pressure was 4 mmHg and portosystemic gradient (PSG) was 20 mmHg, Liver biopsy showed obliterative portal venopathy without liver nodularity or fibrosis (Figure 1c-f). The diagnosis of oxaliplatin induced portosinusoidal vascular disease was made. Large volume rectal bleeding reoccurred on four instances in the following weeks, managed by cautery, hemoclips, and hemostatic spray, all to no avail. Non-occlusive SMV thrombus was also newly discovered on CT angiography. To control bleeding via reducing pressure in the portal system, transjugular intrahepatic portosystemic shunt placement was trialed but unsuccessful due to difficulties with accessing the portal vasculature. Subsequently, direct intrahepatic portocaval shunt was placed with a final PSG of 8mmHg and bleeding was controlled.
Discussion: Clinical presentation of NCPH has been reported to occur within a year of oxaliplatin exposure characterized by variceal bleeding, splenomegaly, or ascites with several underlying mechanisms proposed. Management of this condition follows the same guidelines as management of cirrhotic portal hypertension and cessation of oxaliplatin therapy. This case highlights the importance of vigilance for long-term complications in colon cancer patients treated with this agent.

Figure: Figure 1. A) shows evidence of a prior end-to-end colo-colonic anastomosis in the rectum characterized by congestion, erosion friable mucosa with and actively bleeding site. B) . One erosion with adherent clot treated with hemoclip. C&D) H&E stained liver biopsy sample showing portal tract with loss of portal vein. C&D) Trichrome stained liver samples showing the same in addition to injured and therefore congested and early fibrotic sinusoids, associated with atrophy of hepatocytes.
Disclosures:
Pavithra Ramakrishnan indicated no relevant financial relationships.
Bryant Megna indicated no relevant financial relationships.
Kawthar Mohamed indicated no relevant financial relationships.
Oyedele Adeyi indicated no relevant financial relationships.
Julie Thompson indicated no relevant financial relationships.
Pavithra Ramakrishnan, MS, MD1, Bryant Megna, MD2, Kawthar Mohamed, MD2, Oyedele Adeyi, MD3, Julie Thompson, MD2. P3960 - The Cost of Curing Colon Cancer: Oxaliplatin-Induced NCPH-Related Colonic Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
