Tuesday Poster Session
Category: Liver
P3972 - An Unusual Case of Congestive Hepatopathy Masquerading as Dubin-Johnson Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- JK
Jeong Hoon Kim, MD
University of Pittsburgh Medical Center, Weill Cornell Medical College
Pittsburgh, PA
Presenting Author(s)
Jeong Hoon Kim, MD1, Benjamin Gordon, MD2, Aiya Aboubakr, MD3, Catherine Lucero, MD4, Arun Jesudian, MD5, Anthony Choi, MD5, David Wan, BS, MD5
1University of Pittsburgh Medical Center, Weill Cornell Medical College, Pittsburgh, PA; 2New York Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3New York Presbyterian-Weill Cornell Medical Center, New York, NY; 4Weill Cornell, New York, NY; 5Weill Cornell Medicine, New York, NY
Introduction: Congestive hepatopathy (CH) is hepatocyte injury secondary to increased central venous pressure from right heart failure. It typically causes mild hyperbilirubinemia (total bilirubin < 3). In cases of marked hyperbilirubinemia with no intrinsic liver pathology, concurrent defect in bilirubin metabolism may be suspected. This case featured hyperbilirubinemia with 71% coproporphyrin (CP) I initially attributed to CH with underlying Dubin-Johnson syndrome (DJS) but was later found to be CH alone.
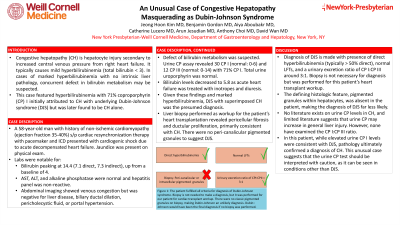
Case Description/Methods: A 58-year-old man with history of non-ischemic cardiomyopathy (ejection fraction 35-40%) s/p cardiac resynchronization therapy with pacemaker and ICD presented with cardiogenic shock due to acute decompensated heart failure. Jaundice was present on physical exam. Labs were notable for bilirubin peaking at 14.4 (7.1 direct, 7.3 indirect), up from a baseline of 4. AST, ALT, and alkaline phosphatase were normal and hepatitis panel was non-reactive. Abdominal imaging showed venous congestion but was negative for liver disease, biliary ductal dilation, pericholecystic fluid, or portal hypertension. Defect of bilirubin metabolism was suspected. Urine CP assay revealed 30 CP I (normal: 0-6) and 12 CP III (normal: 0-14) with 71% CP I. Total urine uroporphyrin was normal. Bilirubin levels decreased to 5.8 as acute heart failure was treated with inotropes and diuresis. Given these findings and marked hyperbilirubinemia, DJS with superimposed CH was the presumed diagnosis. Liver biopsy performed as workup for the patient’s heart transplantation revealed pericellular fibrosis and ductular proliferation, primarily consistent with CH. There were no peri-canalicular pigmented granules to suggest DJS.
Discussion: Diagnosis of DJS is made with presence of direct hyperbilirubinemia (typically > 50% direct), normal LFTs, and a urinary excretion ratio of CP I:CP III around 3:1. The defining histologic feature, pigmented granules within hepatocytes, was absent in the patient, making the diagnosis of DJS far less likely. No literature exists on urine CP levels in CH, and limited literature suggests that urine CP may increase in general liver injury. However, none have examined the CP I:CP III ratio. In this patient, while elevated urine CP I levels were consistent with DJS, pathology ultimately confirmed a diagnosis of CH. This unusual case suggests that the urine CP test should be interpreted with caution, as it can be seen in conditions other than DJS.
Disclosures:
Jeong Hoon Kim, MD1, Benjamin Gordon, MD2, Aiya Aboubakr, MD3, Catherine Lucero, MD4, Arun Jesudian, MD5, Anthony Choi, MD5, David Wan, BS, MD5. P3972 - An Unusual Case of Congestive Hepatopathy Masquerading as Dubin-Johnson Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Weill Cornell Medical College, Pittsburgh, PA; 2New York Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3New York Presbyterian-Weill Cornell Medical Center, New York, NY; 4Weill Cornell, New York, NY; 5Weill Cornell Medicine, New York, NY
Introduction: Congestive hepatopathy (CH) is hepatocyte injury secondary to increased central venous pressure from right heart failure. It typically causes mild hyperbilirubinemia (total bilirubin < 3). In cases of marked hyperbilirubinemia with no intrinsic liver pathology, concurrent defect in bilirubin metabolism may be suspected. This case featured hyperbilirubinemia with 71% coproporphyrin (CP) I initially attributed to CH with underlying Dubin-Johnson syndrome (DJS) but was later found to be CH alone.
Case Description/Methods: A 58-year-old man with history of non-ischemic cardiomyopathy (ejection fraction 35-40%) s/p cardiac resynchronization therapy with pacemaker and ICD presented with cardiogenic shock due to acute decompensated heart failure. Jaundice was present on physical exam. Labs were notable for bilirubin peaking at 14.4 (7.1 direct, 7.3 indirect), up from a baseline of 4. AST, ALT, and alkaline phosphatase were normal and hepatitis panel was non-reactive. Abdominal imaging showed venous congestion but was negative for liver disease, biliary ductal dilation, pericholecystic fluid, or portal hypertension. Defect of bilirubin metabolism was suspected. Urine CP assay revealed 30 CP I (normal: 0-6) and 12 CP III (normal: 0-14) with 71% CP I. Total urine uroporphyrin was normal. Bilirubin levels decreased to 5.8 as acute heart failure was treated with inotropes and diuresis. Given these findings and marked hyperbilirubinemia, DJS with superimposed CH was the presumed diagnosis. Liver biopsy performed as workup for the patient’s heart transplantation revealed pericellular fibrosis and ductular proliferation, primarily consistent with CH. There were no peri-canalicular pigmented granules to suggest DJS.
Discussion: Diagnosis of DJS is made with presence of direct hyperbilirubinemia (typically > 50% direct), normal LFTs, and a urinary excretion ratio of CP I:CP III around 3:1. The defining histologic feature, pigmented granules within hepatocytes, was absent in the patient, making the diagnosis of DJS far less likely. No literature exists on urine CP levels in CH, and limited literature suggests that urine CP may increase in general liver injury. However, none have examined the CP I:CP III ratio. In this patient, while elevated urine CP I levels were consistent with DJS, pathology ultimately confirmed a diagnosis of CH. This unusual case suggests that the urine CP test should be interpreted with caution, as it can be seen in conditions other than DJS.
Disclosures:
Jeong Hoon Kim indicated no relevant financial relationships.
Benjamin Gordon indicated no relevant financial relationships.
Aiya Aboubakr indicated no relevant financial relationships.
Catherine Lucero indicated no relevant financial relationships.
Arun Jesudian: Dynavax Therapeutics – Speakers Bureau. Salix Pharmaceuticals – Consultant, Speakers Bureau.
Anthony Choi indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Jeong Hoon Kim, MD1, Benjamin Gordon, MD2, Aiya Aboubakr, MD3, Catherine Lucero, MD4, Arun Jesudian, MD5, Anthony Choi, MD5, David Wan, BS, MD5. P3972 - An Unusual Case of Congestive Hepatopathy Masquerading as Dubin-Johnson Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

