Tuesday Poster Session
Category: Liver
P4013 - Acquired Hepatocerebral Degeneration and Chronic Liver Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ereny Demian, MD
Penn State College of Medicine
Hershey, PA
Presenting Author(s)
Ereny Demian, MD, Papul Chalia, MD, Sol De Jesus, MD
Penn State College of Medicine, Hershey, PA
Introduction: Acquired hepatocerebral degeneration (AHD) is a rare neurological syndrome in patients with chronic liver disease, particularly involving portosystemic shunts. MRI findings include T1 hyperintensity in basal ganglia structures and periaqueductal gray matter2. AHD is an underdiagnosed condition with limited treatment options. We report a case of a 54-year-old female who presents with altered mental status (AMS) and hyperkinetic movement disorders in the setting of Budd Chiari Syndrome status post TIPS and recurrent hepatic encephalopathy (HE).
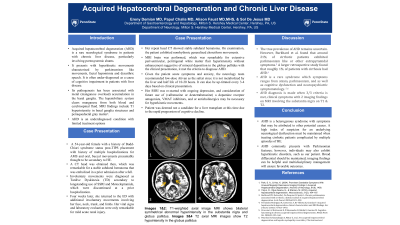
Case Description/Methods: Patient is a 54-year-old female with a history of Budd-Chiari syndrome status post-TIPS placement. Patient first presented to our ED four weeks earlier with symptoms of AMS and oral, buccal movements presumably thought to be secondary to HE. A CT head was obtained, which was remarkable for a stable subdural hematoma that was embolized in a prior admission after a fall. Involuntary movements were diagnosed as Tardive Dyskinesia (TD) secondary to longstanding use of SSRI and Metoclopramide, which were discontinued at discharge. Four weeks later, she returned to the ED with additional involuntary movements involving her face, neck, trunk, and limbs. Her vital signs and laboratory evaluation were only remarkable for mild acute renal injury. Her repeat head CT showed stable subdural hematoma. On examination, the patient exhibited nonrhythmic generalized choreiform movements. MRI brain was performed, which was remarkable for extensive periventricular, peritrigonal white matter flair hyperintensity without enhancement suggestive of mineral deposition in the globus pallidus. Low-dose Ativan was trialed, which was shown to be effective. She was deemed not a candidate for a liver transplant at this time. Her SSRI was re-started with ongoing depression, and consideration of future use of dopamine receptor antagonists, VMAT inhibitors, and or anticholinergics may be necessary for hyperkinetic movements.
Discussion: AHD is a heterogenous syndrome with symptoms that may be attributed to other potential causes. A high index of suspicion for an underlying neurological dysfunction must be maintained when treating cirrhotic patients complicated by multiple episodes of HE. AHD commonly presents with Parkinsonian features; however, individuals may also exhibit hyperkinetic disorders, such as our patient. Broad differential should be maintained; imaging findings can be helpful and multidisciplinary management will ensure favorable outcomes.

Disclosures:
Ereny Demian, MD, Papul Chalia, MD, Sol De Jesus, MD. P4013 - Acquired Hepatocerebral Degeneration and Chronic Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Penn State College of Medicine, Hershey, PA
Introduction: Acquired hepatocerebral degeneration (AHD) is a rare neurological syndrome in patients with chronic liver disease, particularly involving portosystemic shunts. MRI findings include T1 hyperintensity in basal ganglia structures and periaqueductal gray matter2. AHD is an underdiagnosed condition with limited treatment options. We report a case of a 54-year-old female who presents with altered mental status (AMS) and hyperkinetic movement disorders in the setting of Budd Chiari Syndrome status post TIPS and recurrent hepatic encephalopathy (HE).
Case Description/Methods: Patient is a 54-year-old female with a history of Budd-Chiari syndrome status post-TIPS placement. Patient first presented to our ED four weeks earlier with symptoms of AMS and oral, buccal movements presumably thought to be secondary to HE. A CT head was obtained, which was remarkable for a stable subdural hematoma that was embolized in a prior admission after a fall. Involuntary movements were diagnosed as Tardive Dyskinesia (TD) secondary to longstanding use of SSRI and Metoclopramide, which were discontinued at discharge. Four weeks later, she returned to the ED with additional involuntary movements involving her face, neck, trunk, and limbs. Her vital signs and laboratory evaluation were only remarkable for mild acute renal injury. Her repeat head CT showed stable subdural hematoma. On examination, the patient exhibited nonrhythmic generalized choreiform movements. MRI brain was performed, which was remarkable for extensive periventricular, peritrigonal white matter flair hyperintensity without enhancement suggestive of mineral deposition in the globus pallidus. Low-dose Ativan was trialed, which was shown to be effective. She was deemed not a candidate for a liver transplant at this time. Her SSRI was re-started with ongoing depression, and consideration of future use of dopamine receptor antagonists, VMAT inhibitors, and or anticholinergics may be necessary for hyperkinetic movements.
Discussion: AHD is a heterogenous syndrome with symptoms that may be attributed to other potential causes. A high index of suspicion for an underlying neurological dysfunction must be maintained when treating cirrhotic patients complicated by multiple episodes of HE. AHD commonly presents with Parkinsonian features; however, individuals may also exhibit hyperkinetic disorders, such as our patient. Broad differential should be maintained; imaging findings can be helpful and multidisciplinary management will ensure favorable outcomes.

Figure: MRI Brain/Head with and without Contrast:
Figure 1: T1-weighted axial image MRI shows bilateral symmetrical abnormal hyperintensity in the substanita nigra
Figure 2: T1-weighted axial MRI shows bilateral symmetrical abnormal hyperintensity in the globus pallidus
Figure 1: T1-weighted axial image MRI shows bilateral symmetrical abnormal hyperintensity in the substanita nigra
Figure 2: T1-weighted axial MRI shows bilateral symmetrical abnormal hyperintensity in the globus pallidus
Disclosures:
Ereny Demian indicated no relevant financial relationships.
Papul Chalia indicated no relevant financial relationships.
Sol De Jesus indicated no relevant financial relationships.
Ereny Demian, MD, Papul Chalia, MD, Sol De Jesus, MD. P4013 - Acquired Hepatocerebral Degeneration and Chronic Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

