Tuesday Poster Session
Category: Liver
P4019 - Hepatopulmonary Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Anh Trinh Doan, DO
Baylor Scott & White
Belton, TX
Presenting Author(s)
Anh Trinh Doan, DO1, Ashkan Khosravi, DO2
1Baylor Scott & White, Belton, TX; 2Baylor Scott & White, Temple, TX
Introduction: Hepatopulmonary syndrome (HPS) is an oxygenation defect caused by the development of intrapulmonary vascular dilation in the setting of advanced liver disease. The prevalence of HPS among liver transplant patients ranges from 5-32%. Cirrhotic patients with HPS have two times higher mortality than those with no HPS. To avoid high mortality and morbidity, diagnosing and treating promptly is critical.
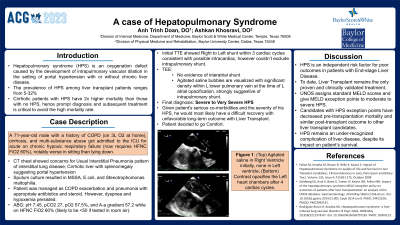
Case Description/Methods: A 71-year-old male with a history of chronic obstructive pulmonary disease (COPD) (on 3L oxygen at home), cirrhosis, alcohol, and nicotine abuse got admitted to Intensive Care Unit for acute on chronic hypoxic respiratory failure, notably worse in sitting than lying down. Initially, the patient was managed as COPD exacerbation and pneumonia with IV ceftriaxone, azithromycin, and prednisone 40mg. CT chest showed concerns for usual interstitial pneumonia pattern of intestinal lung disease. Sputum culture resulted in Stenotrophomonas maltophilia. Minocycline was added. His dyspnea and hypoxemia persisted. ABG revealed pH 7.45, pCO2 27, pO2 57.5, and A-a gradient 57.2 while on 60% HFNC. Transesophageal echocardiogram with bubble study suggested a large Right to Left shunt visualized by agitated saline injection, which opacified the entire Left side. The patient was then diagnosed with severe- very severe hepatopulmonary syndrome.
After diagnosis, a transplant hepatologist was consulted and evaluated the patient as not a good candidate for transplant due to high O2 needs and co-morbidities. Additionally, his MELD score (13-15) would not be high enough for a transplant, even with extra points added due to HPS. The patient passed away 15 days later.
Discussion: The diagnosis and treatment of HPS highlight the role of the interprofessional team approach in care for these complicated patients. HPS diagnosis requires oxygenation defect, intrapulmonary vascular dilatation, and liver disease (with or without portal hypertension). There is no hallmark of HPS in physical exams. However, the presence of severe hypoxemia, spider nevi, digital clubbing, platypnea, and orthodeoxia in the setting of long-term liver disease could be suggestive. The only successful treatment for HPS is a liver transplant. Patients had a 5-year survival rate of 76% after liver transplant, a rate that is not significantly different from that among patients without the HPS who underwent transplantation.
Disclosures:
Anh Trinh Doan, DO1, Ashkan Khosravi, DO2. P4019 - Hepatopulmonary Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baylor Scott & White, Belton, TX; 2Baylor Scott & White, Temple, TX
Introduction: Hepatopulmonary syndrome (HPS) is an oxygenation defect caused by the development of intrapulmonary vascular dilation in the setting of advanced liver disease. The prevalence of HPS among liver transplant patients ranges from 5-32%. Cirrhotic patients with HPS have two times higher mortality than those with no HPS. To avoid high mortality and morbidity, diagnosing and treating promptly is critical.
Case Description/Methods: A 71-year-old male with a history of chronic obstructive pulmonary disease (COPD) (on 3L oxygen at home), cirrhosis, alcohol, and nicotine abuse got admitted to Intensive Care Unit for acute on chronic hypoxic respiratory failure, notably worse in sitting than lying down. Initially, the patient was managed as COPD exacerbation and pneumonia with IV ceftriaxone, azithromycin, and prednisone 40mg. CT chest showed concerns for usual interstitial pneumonia pattern of intestinal lung disease. Sputum culture resulted in Stenotrophomonas maltophilia. Minocycline was added. His dyspnea and hypoxemia persisted. ABG revealed pH 7.45, pCO2 27, pO2 57.5, and A-a gradient 57.2 while on 60% HFNC. Transesophageal echocardiogram with bubble study suggested a large Right to Left shunt visualized by agitated saline injection, which opacified the entire Left side. The patient was then diagnosed with severe- very severe hepatopulmonary syndrome.
After diagnosis, a transplant hepatologist was consulted and evaluated the patient as not a good candidate for transplant due to high O2 needs and co-morbidities. Additionally, his MELD score (13-15) would not be high enough for a transplant, even with extra points added due to HPS. The patient passed away 15 days later.
Discussion: The diagnosis and treatment of HPS highlight the role of the interprofessional team approach in care for these complicated patients. HPS diagnosis requires oxygenation defect, intrapulmonary vascular dilatation, and liver disease (with or without portal hypertension). There is no hallmark of HPS in physical exams. However, the presence of severe hypoxemia, spider nevi, digital clubbing, platypnea, and orthodeoxia in the setting of long-term liver disease could be suggestive. The only successful treatment for HPS is a liver transplant. Patients had a 5-year survival rate of 76% after liver transplant, a rate that is not significantly different from that among patients without the HPS who underwent transplantation.
Disclosures:
Anh Trinh Doan indicated no relevant financial relationships.
Ashkan Khosravi indicated no relevant financial relationships.
Anh Trinh Doan, DO1, Ashkan Khosravi, DO2. P4019 - Hepatopulmonary Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
