Tuesday Poster Session
Category: Liver
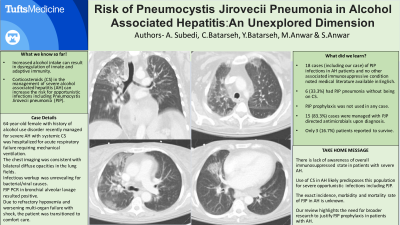
P4021 - Risk of Pneumocystis Jirovecii Pneumonia in Alcohol-Associated Hepatitis- An Unexplored Dimension
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- SA
Shamsuddin Anwar, MD
Tufts Medical Center
Quincy, MA
Presenting Author(s)
Ankita Subedi, MD, MBBS1, Cristina Batarseh, MD2, Yazan Batarseh, PharmD, PhD3, Mahreen Anwar, 4, Shamsuddin Anwar, MD5
1Tufts Medical Center, Boston, MA; 2Lahey Hospital and Medical Center, Boston, MA; 3Lemuel Shattuck Hospital, Boston, MA; 4Central Michigan University, Mount Pleasant, MI; 5Tufts Medical Center, Quincy, MA
Introduction: Alcohol associated Hepatitis (AH) is a form of liver inflammation associated with excessive alcohol consumption. Evidence suggests complex interaction of alcohol intake with the dysregulation of innate and adaptive immunity predisposing opportunistic infections. Patients with AH have greater T cell suppression compared to chronically stable advanced liver diseases. Corticosteroids (CS) are used in the management of severe AH to reduce the short term mortality but high dose ( >30 milligrams/day) and longer duration ( >4 weeks) of CS can increase the risk for opportunistic infections including Pneumocystis Jirovecii pneumonia (PJP). To our knowledge, there are no definite guidelines to suggest PJP prophylaxis in patients managed with CS for AH.
Case Description/Methods: We present a case of a 64-year-old female with history of alcohol use disorder who was managed for severe AH with systemic CS. Soon after finishing the CS course, the patient was hospitalized for a mechanical fall evaluation complicated with rapid clinical deterioration and acute respiratory failure requiring mechanical ventilation. The chest imaging was consistent with bilateral diffuse opacities in the lung fields; however, no overt cause of respiratory failure was determined. Infectious workup was unrevealing for bacterial causes while she remained on broad spectrum antibiotics. Due to refractory hypoxemia and worsening multi-organ failure with shock, the patient was transitioned to comfort care and deceased on the fourth day of hospitalization. On the sixth day, the PJP PCR in the bronchial alveolar lavage returned positive.
Discussion: We found 13 cases in medical literature of PJP pneumonia with AH and no other immunosuppressed status. None were on PJP prophylaxis. Two cases had PJP pneumonia even without being treated with CS. There is paucity of data if patients with AH are more predisposed to PJP pneumonia or the use of CS increases the risk. This could be due to lack of awareness about the overall immunosuppressed state in patients with severe AH. With the increasing prevalence of alcohol use disorder and AH, the management of these individuals should also include risk assessment for opportunistic and fatal infections like PJP. This review highlights these unique requirements for patients with severe alcohol associated hepatitis. With the data presented here we hope to open venues for further research to evaluate the role of PJP prophylaxis in patients with AH, especially who were given systemic CS.

Disclosures:
Ankita Subedi, MD, MBBS1, Cristina Batarseh, MD2, Yazan Batarseh, PharmD, PhD3, Mahreen Anwar, 4, Shamsuddin Anwar, MD5. P4021 - Risk of Pneumocystis Jirovecii Pneumonia in Alcohol-Associated Hepatitis- An Unexplored Dimension, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Lahey Hospital and Medical Center, Boston, MA; 3Lemuel Shattuck Hospital, Boston, MA; 4Central Michigan University, Mount Pleasant, MI; 5Tufts Medical Center, Quincy, MA
Introduction: Alcohol associated Hepatitis (AH) is a form of liver inflammation associated with excessive alcohol consumption. Evidence suggests complex interaction of alcohol intake with the dysregulation of innate and adaptive immunity predisposing opportunistic infections. Patients with AH have greater T cell suppression compared to chronically stable advanced liver diseases. Corticosteroids (CS) are used in the management of severe AH to reduce the short term mortality but high dose ( >30 milligrams/day) and longer duration ( >4 weeks) of CS can increase the risk for opportunistic infections including Pneumocystis Jirovecii pneumonia (PJP). To our knowledge, there are no definite guidelines to suggest PJP prophylaxis in patients managed with CS for AH.
Case Description/Methods: We present a case of a 64-year-old female with history of alcohol use disorder who was managed for severe AH with systemic CS. Soon after finishing the CS course, the patient was hospitalized for a mechanical fall evaluation complicated with rapid clinical deterioration and acute respiratory failure requiring mechanical ventilation. The chest imaging was consistent with bilateral diffuse opacities in the lung fields; however, no overt cause of respiratory failure was determined. Infectious workup was unrevealing for bacterial causes while she remained on broad spectrum antibiotics. Due to refractory hypoxemia and worsening multi-organ failure with shock, the patient was transitioned to comfort care and deceased on the fourth day of hospitalization. On the sixth day, the PJP PCR in the bronchial alveolar lavage returned positive.
Discussion: We found 13 cases in medical literature of PJP pneumonia with AH and no other immunosuppressed status. None were on PJP prophylaxis. Two cases had PJP pneumonia even without being treated with CS. There is paucity of data if patients with AH are more predisposed to PJP pneumonia or the use of CS increases the risk. This could be due to lack of awareness about the overall immunosuppressed state in patients with severe AH. With the increasing prevalence of alcohol use disorder and AH, the management of these individuals should also include risk assessment for opportunistic and fatal infections like PJP. This review highlights these unique requirements for patients with severe alcohol associated hepatitis. With the data presented here we hope to open venues for further research to evaluate the role of PJP prophylaxis in patients with AH, especially who were given systemic CS.

Figure: Computed tomographic (CT) images of the chest
Disclosures:
Ankita Subedi indicated no relevant financial relationships.
Cristina Batarseh indicated no relevant financial relationships.
Yazan Batarseh indicated no relevant financial relationships.
Mahreen Anwar indicated no relevant financial relationships.
Shamsuddin Anwar indicated no relevant financial relationships.
Ankita Subedi, MD, MBBS1, Cristina Batarseh, MD2, Yazan Batarseh, PharmD, PhD3, Mahreen Anwar, 4, Shamsuddin Anwar, MD5. P4021 - Risk of Pneumocystis Jirovecii Pneumonia in Alcohol-Associated Hepatitis- An Unexplored Dimension, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
