Tuesday Poster Session
Category: Obesity
P4025 - Bariatric Surgery Has Differential Effects on the Risk of De Novo Inflammatory Bowel Disease, Depending on Type and the Length of the Follow-Up After Surgery
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Antoinette J. Pusateri, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Antoinette J. Pusateri, MD1, Kenneth Allen, DO1, Yevgeniya Gokun, MS1, ChienWei Chiang, PhD2, Adeeti Chiplunker, MD, MMS1, Madalina Butnariu, MD3, Hisham Hussan, MD4
1The Ohio State University Wexner Medical Center, Columbus, OH; 2College of Medicine, The Ohio State University, Columbus, OH; 3The Ohio State University, Columbus, OH; 4Gastroenterology & Hepatology, University of California Davis Health, Sacramento, CA
Introduction: Obesity may promote the development of inflammatory bowel disease (IBD) in genetically predisposed individuals. Weight loss after bariatric surgery (BRS) should reduce the risk and severity of IBD. However, BRS also induces intestinal microbiome-metabolome changes (e.g., increased E. coli and reduced butyrate) that can influence the risk of future IBD. We aimed to assess the risk and severity of new IBD in severely obese adults with and without BRS.
Methods: This retrospective cohort study used the 2012-2020 MarketScan database. Adults with severe obesity were propensity score-matched based on the presence or absence of BRS – Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (VSG). Our strict eligibility criteria were notable for excluding immunosuppression, IBD or IBD medications' use before surgery or obesity documentation. IBD was defined using a precise, validated coding (multiple IBD visits and use of IBD medications). We examined IBD risk < 3 or ≥3 years from BRS compared to severe obesity after adjusting for important covariates. Significance was defined as p< 0.05.
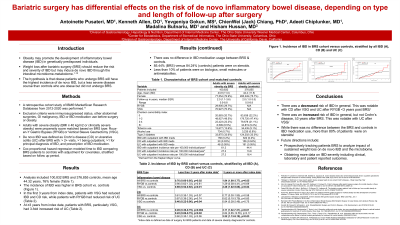
Results: Our analysis included 100,832 BRS and 376,855 controls with severe obesity (mean age of 44.32, 76% female). The incidence of IBD was higher in the BRS cohort vs. controls (61.2 vs. 44.4 per 100,000 individuals, KM curves in Fig. 1). Adults with BRS had a 24% lower risk of developing IBD and a 51% lower risk of ulcerative colitis than controls in the first 3 years (Table 1). When stratified by BRS type, VSG was associated with reduced IBD risk, mainly Crohn’s disease, in the first 3 years post-surgery (HR: 0.46, 95%CI: 0.22-0.96), while RYGB subjects were at lower risk of ulcerative colitis (HR: 0.22, 95%CI: 0.06-0.75). Paradoxically, at ≥3 years, adults with BRS were at higher risk for new IBD than controls. Specifically, BRS, especially VSG, was associated with a 3-fold higher risk of ulcerative colitis (HR: 3.22, 95%CI: 1.13-9.19). In adults with new IBD, there were no significant differences in the use of steroids (85.4% vs. 84.2%, p=0.71), biologics/small molecules (5.1% vs 8.2%, p=0.18), or antimetabolites (8.2% vs. 8.5%, p=0.91) between the BRS and controls with new IBD.
Discussion: The risk of newly diagnosed IBD is reduced < 3 years after BRS but paradoxically increased at 3 years or more after BRS, especially ulcerative colitis after VSG. Further mechanistic research is needed to elucidate the long-term effects of BRS-induced microbiome changes on IBD risk.

Disclosures:
Antoinette J. Pusateri, MD1, Kenneth Allen, DO1, Yevgeniya Gokun, MS1, ChienWei Chiang, PhD2, Adeeti Chiplunker, MD, MMS1, Madalina Butnariu, MD3, Hisham Hussan, MD4. P4025 - Bariatric Surgery Has Differential Effects on the Risk of De Novo Inflammatory Bowel Disease, Depending on Type and the Length of the Follow-Up After Surgery, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2College of Medicine, The Ohio State University, Columbus, OH; 3The Ohio State University, Columbus, OH; 4Gastroenterology & Hepatology, University of California Davis Health, Sacramento, CA
Introduction: Obesity may promote the development of inflammatory bowel disease (IBD) in genetically predisposed individuals. Weight loss after bariatric surgery (BRS) should reduce the risk and severity of IBD. However, BRS also induces intestinal microbiome-metabolome changes (e.g., increased E. coli and reduced butyrate) that can influence the risk of future IBD. We aimed to assess the risk and severity of new IBD in severely obese adults with and without BRS.
Methods: This retrospective cohort study used the 2012-2020 MarketScan database. Adults with severe obesity were propensity score-matched based on the presence or absence of BRS – Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (VSG). Our strict eligibility criteria were notable for excluding immunosuppression, IBD or IBD medications' use before surgery or obesity documentation. IBD was defined using a precise, validated coding (multiple IBD visits and use of IBD medications). We examined IBD risk < 3 or ≥3 years from BRS compared to severe obesity after adjusting for important covariates. Significance was defined as p< 0.05.
Results: Our analysis included 100,832 BRS and 376,855 controls with severe obesity (mean age of 44.32, 76% female). The incidence of IBD was higher in the BRS cohort vs. controls (61.2 vs. 44.4 per 100,000 individuals, KM curves in Fig. 1). Adults with BRS had a 24% lower risk of developing IBD and a 51% lower risk of ulcerative colitis than controls in the first 3 years (Table 1). When stratified by BRS type, VSG was associated with reduced IBD risk, mainly Crohn’s disease, in the first 3 years post-surgery (HR: 0.46, 95%CI: 0.22-0.96), while RYGB subjects were at lower risk of ulcerative colitis (HR: 0.22, 95%CI: 0.06-0.75). Paradoxically, at ≥3 years, adults with BRS were at higher risk for new IBD than controls. Specifically, BRS, especially VSG, was associated with a 3-fold higher risk of ulcerative colitis (HR: 3.22, 95%CI: 1.13-9.19). In adults with new IBD, there were no significant differences in the use of steroids (85.4% vs. 84.2%, p=0.71), biologics/small molecules (5.1% vs 8.2%, p=0.18), or antimetabolites (8.2% vs. 8.5%, p=0.91) between the BRS and controls with new IBD.
Discussion: The risk of newly diagnosed IBD is reduced < 3 years after BRS but paradoxically increased at 3 years or more after BRS, especially ulcerative colitis after VSG. Further mechanistic research is needed to elucidate the long-term effects of BRS-induced microbiome changes on IBD risk.

Figure: Figure 1. Incidence of inflammatory bowel disease (IBD) in the bariatric surgery (BRS) cohort versus controls, stratified by all IBD (A), Crohn’s disease (B) and ulcerative colitis (C)
Disclosures:
Antoinette Pusateri indicated no relevant financial relationships.
Kenneth Allen indicated no relevant financial relationships.
Yevgeniya Gokun indicated no relevant financial relationships.
ChienWei Chiang indicated no relevant financial relationships.
Adeeti Chiplunker indicated no relevant financial relationships.
Madalina Butnariu indicated no relevant financial relationships.
Hisham Hussan indicated no relevant financial relationships.
Antoinette J. Pusateri, MD1, Kenneth Allen, DO1, Yevgeniya Gokun, MS1, ChienWei Chiang, PhD2, Adeeti Chiplunker, MD, MMS1, Madalina Butnariu, MD3, Hisham Hussan, MD4. P4025 - Bariatric Surgery Has Differential Effects on the Risk of De Novo Inflammatory Bowel Disease, Depending on Type and the Length of the Follow-Up After Surgery, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
