Tuesday Poster Session
Category: Practice Management
P4047 - Impact of an Electronic Smart Order-Set on Clostridiodes Difficile Infection Testing in a Community Healthcare System in South Florida
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Shiv Krishnaswamy, MD
Memorial Healthcare System
Fort Lauderdale, FL
Presenting Author(s)
Ayesha T. Jalal, MD1, Elsa Acevedo Martinez, MD1, Shiv Krishnaswamy, MD1, Rachel Guran, PhD1, Shenae Samuels, PhD1, Ajay Desai, BS2, Nancimae Miller, PhD1, Paula Eckardt, MD1
1Memorial Healthcare System, Hollywood, FL; 2Florida Atlantic University, Hollywood, FL
Introduction: SHEA/IDSA/APIC practice recommendations for acute-care hospitals to prevent<span class="s1"> Clostridiodes difficile infection (CDI)</span> is the implementation of diagnostic stewardship practices including appropriate use of testing. In order to avoid CDI testing in patients without clinically significant diarrhea (3 or more watery or loose stools in 24 hours), our study leveraged the EMR system for a computerized provider order entry hard stop through an electronic C. difficile order set (ECOS) in patients that had laxatives within 48 hours of ordering a C. difficile test and a prompt for clinical criteria.
Methods: A retrospective chart review of patients who were tested for CDI, before and after implementation of a smart ECOS was conducted. Records whose samples were canceled by the lab for inappropriate specimens, and patients < 18 years or pregnant were excluded. Pre-intervention period spanned March 13, 2021 to February 22, 2022 and post-intervention period spanned February 23, 2022, to December 31, 2022. The primary aim of the study was to determine if the rate of inappropriate stool testing for CDI changed pre- and post-implementation of an ECOS, as well as to determine if there was a significant change in secondary outcomes of interest.
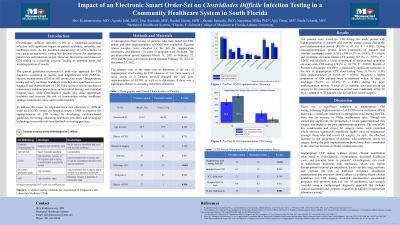
Results: 224 patients were tested for CDI during the study period with higher proportion of patients who met the testing criteria during the post-implementation period (80.5% vs. 61.3%; P = 0.002). During post-implementation period: lower proportion of patients had absolute neutrophil count (ANC) < /=500 (5.1% vs. 10.4%; P = 0.019) and creatinine elevation before CDI testing (33.1% vs. 50.9%; P = 0.007) and similarly a lower proportion of patients had creatinine elevation after CDI testing (29.1% vs. 43.7%; P = 0.030). Results of the Pearson’s chi-square test show a statistically significant reduction in the rate of inappropriate stool testing for CDI from 31.1% to 11.0% after implementation of ECOS (P < 0.001). However, a higher proportion of CDI patients were re-admitted within 30 days of discharge (54.2% vs. 33.0%; P = 0.001) during the post-implementation period.
Discussion: There was a significant reduction in inappropriate stool testing for CDI following the implementation of ECOS at our institution. During the post-intervention period, an increase in 30-day readmission rates was observed. Likewise, the proportion of recent gastrointestinal (GI) surgery was higher in this period, which could have contributed to the readmission rate.

Disclosures:
Ayesha T. Jalal, MD1, Elsa Acevedo Martinez, MD1, Shiv Krishnaswamy, MD1, Rachel Guran, PhD1, Shenae Samuels, PhD1, Ajay Desai, BS2, Nancimae Miller, PhD1, Paula Eckardt, MD1. P4047 - Impact of an Electronic Smart Order-Set on Clostridiodes Difficile Infection Testing in a Community Healthcare System in South Florida, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Memorial Healthcare System, Hollywood, FL; 2Florida Atlantic University, Hollywood, FL
Introduction: SHEA/IDSA/APIC practice recommendations for acute-care hospitals to prevent<span class="s1"> Clostridiodes difficile infection (CDI)</span> is the implementation of diagnostic stewardship practices including appropriate use of testing. In order to avoid CDI testing in patients without clinically significant diarrhea (3 or more watery or loose stools in 24 hours), our study leveraged the EMR system for a computerized provider order entry hard stop through an electronic C. difficile order set (ECOS) in patients that had laxatives within 48 hours of ordering a C. difficile test and a prompt for clinical criteria.
Methods: A retrospective chart review of patients who were tested for CDI, before and after implementation of a smart ECOS was conducted. Records whose samples were canceled by the lab for inappropriate specimens, and patients < 18 years or pregnant were excluded. Pre-intervention period spanned March 13, 2021 to February 22, 2022 and post-intervention period spanned February 23, 2022, to December 31, 2022. The primary aim of the study was to determine if the rate of inappropriate stool testing for CDI changed pre- and post-implementation of an ECOS, as well as to determine if there was a significant change in secondary outcomes of interest.
Results: 224 patients were tested for CDI during the study period with higher proportion of patients who met the testing criteria during the post-implementation period (80.5% vs. 61.3%; P = 0.002). During post-implementation period: lower proportion of patients had absolute neutrophil count (ANC) < /=500 (5.1% vs. 10.4%; P = 0.019) and creatinine elevation before CDI testing (33.1% vs. 50.9%; P = 0.007) and similarly a lower proportion of patients had creatinine elevation after CDI testing (29.1% vs. 43.7%; P = 0.030). Results of the Pearson’s chi-square test show a statistically significant reduction in the rate of inappropriate stool testing for CDI from 31.1% to 11.0% after implementation of ECOS (P < 0.001). However, a higher proportion of CDI patients were re-admitted within 30 days of discharge (54.2% vs. 33.0%; P = 0.001) during the post-implementation period.
Discussion: There was a significant reduction in inappropriate stool testing for CDI following the implementation of ECOS at our institution. During the post-intervention period, an increase in 30-day readmission rates was observed. Likewise, the proportion of recent gastrointestinal (GI) surgery was higher in this period, which could have contributed to the readmission rate.

Figure: Proportions for inappropriate stool testing status and 30-day readmission status with 95% confidence interval (CI) are presented confirming statistically significant differences between the pre- and post-implementation periods of the study.
Disclosures:
Ayesha Jalal indicated no relevant financial relationships.
Elsa Acevedo Martinez indicated no relevant financial relationships.
Shiv Krishnaswamy indicated no relevant financial relationships.
Rachel Guran indicated no relevant financial relationships.
Shenae Samuels indicated no relevant financial relationships.
Ajay Desai indicated no relevant financial relationships.
Nancimae Miller indicated no relevant financial relationships.
Paula Eckardt indicated no relevant financial relationships.
Ayesha T. Jalal, MD1, Elsa Acevedo Martinez, MD1, Shiv Krishnaswamy, MD1, Rachel Guran, PhD1, Shenae Samuels, PhD1, Ajay Desai, BS2, Nancimae Miller, PhD1, Paula Eckardt, MD1. P4047 - Impact of an Electronic Smart Order-Set on Clostridiodes Difficile Infection Testing in a Community Healthcare System in South Florida, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
