Tuesday Poster Session
Category: Practice Management
P4081 - The Impact of Language in Utilization of Upper Endoscopy for Diagnosis of Functional Dyspepsia
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Noor Siddiqi Syed, MD
Santa Clara Valley Medical Center
Saratoga, CA
Presenting Author(s)
Noor Syed, MD1, Ahmad Kamal, MD2, Linda Anh Nguyen, MD3
1Santa Clara Valley Medical Center, Saratoga, CA; 2Santa Clara Valley Medical Center, San Jose, CA; 3Stanford University, Redwood City, CA
Introduction: Functional dyspepsia (FD) is a disorder of gut-brain interaction (DGBI) characterized by recurring abdominal pain and indigestion. Studies of healthcare utilization in patients with irritable bowel syndrome (IBS) have found that those who self-identify as “Hispanic,” “Black” or “Asian” are more likely to undergo invasive procedures than matched “White” patients with IBS. However, the impact of a patient's preferred language on risk of undergoing procedures is unknown. Since communication and education are key components of FD treatment, we investigated whether non-English speaking patients were more likely to undergo an invasive work-up.
Methods: We retrospectively reviewed charts of 160 patients with a diagnosis of FD in a large public health system serving a diverse population. We excluded patients under age 18, or with a history of peptic ulcer disease, gastric cancer, gastric surgery, or alarm symptoms. Our primary outcome was having had an upper endoscopy as part of FD work-up. Data were analyzed using Pearson’s chi square test with Yates’ continuity correction for categorical data, and Student’s unpaired t-test for continuous data. Logistic regression was used to correct for the impact of covariates. All p-values are 2-sided. Tests were implemented on R version 4.3.0.
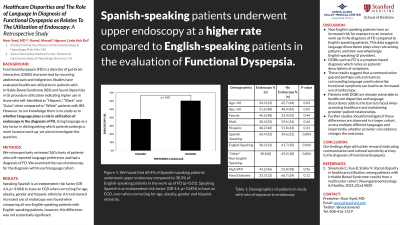
Results: Fifty-three patients reported Spanish as their primary language; 82 reported English, and 26 reported another language (Table 1). Spanish-speaking patients underwent upper endoscopy at a higher rate in the evaluation of FD (60% vs. 36%, p = 0.004). After correcting for age, gender, obesity, diabetes and Hispanic ethnicity, being a Spanish speaker remained an independent risk factor for undergoing EGD (OR 3.9, p= 0.008). We did not see increased utilization of EGD in the “other” language group compared to English speakers.
Discussion: FD is a diagnosis which relies on patients' descriptions of symptoms that meet diagnostic criteria developed in English. These results suggest that a communication gap and perhaps cultural nuances may lead to uncertainty around the diagnosis and a resultant increased use of endoscopy. The lack of difference in EGD utilization in the “other” language group was likely due to a small sample size. Further studies should investigate if these differences are observed in a larger cohort, across multiple different languages and importantly, whether provider language concordance changes the outcomes.
Disclosures:
Noor Syed, MD1, Ahmad Kamal, MD2, Linda Anh Nguyen, MD3. P4081 - The Impact of Language in Utilization of Upper Endoscopy for Diagnosis of Functional Dyspepsia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Santa Clara Valley Medical Center, Saratoga, CA; 2Santa Clara Valley Medical Center, San Jose, CA; 3Stanford University, Redwood City, CA
Introduction: Functional dyspepsia (FD) is a disorder of gut-brain interaction (DGBI) characterized by recurring abdominal pain and indigestion. Studies of healthcare utilization in patients with irritable bowel syndrome (IBS) have found that those who self-identify as “Hispanic,” “Black” or “Asian” are more likely to undergo invasive procedures than matched “White” patients with IBS. However, the impact of a patient's preferred language on risk of undergoing procedures is unknown. Since communication and education are key components of FD treatment, we investigated whether non-English speaking patients were more likely to undergo an invasive work-up.
Methods: We retrospectively reviewed charts of 160 patients with a diagnosis of FD in a large public health system serving a diverse population. We excluded patients under age 18, or with a history of peptic ulcer disease, gastric cancer, gastric surgery, or alarm symptoms. Our primary outcome was having had an upper endoscopy as part of FD work-up. Data were analyzed using Pearson’s chi square test with Yates’ continuity correction for categorical data, and Student’s unpaired t-test for continuous data. Logistic regression was used to correct for the impact of covariates. All p-values are 2-sided. Tests were implemented on R version 4.3.0.
Results: Fifty-three patients reported Spanish as their primary language; 82 reported English, and 26 reported another language (Table 1). Spanish-speaking patients underwent upper endoscopy at a higher rate in the evaluation of FD (60% vs. 36%, p = 0.004). After correcting for age, gender, obesity, diabetes and Hispanic ethnicity, being a Spanish speaker remained an independent risk factor for undergoing EGD (OR 3.9, p= 0.008). We did not see increased utilization of EGD in the “other” language group compared to English speakers.
Discussion: FD is a diagnosis which relies on patients' descriptions of symptoms that meet diagnostic criteria developed in English. These results suggest that a communication gap and perhaps cultural nuances may lead to uncertainty around the diagnosis and a resultant increased use of endoscopy. The lack of difference in EGD utilization in the “other” language group was likely due to a small sample size. Further studies should investigate if these differences are observed in a larger cohort, across multiple different languages and importantly, whether provider language concordance changes the outcomes.
Disclosures:
Noor Syed indicated no relevant financial relationships.
Ahmad Kamal indicated no relevant financial relationships.
Linda Anh Nguyen: Ardelyx – Consultant. Atmo Biosciences – Consultant. Bold Health – Grant/Research Support. Evoke – Consultant. Gemelli – Consultant. Impel – Consultant. Neurogastryx – Consultant. Pendulum – Consultant. Phathom – Consultant. RosVivo – Advisor or Review Panel Member. Takeda – Consultant.
Noor Syed, MD1, Ahmad Kamal, MD2, Linda Anh Nguyen, MD3. P4081 - The Impact of Language in Utilization of Upper Endoscopy for Diagnosis of Functional Dyspepsia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
