Tuesday Poster Session
Category: Practice Management
P4096 - Association of Social Determinants of Health With Late-Stage Diagnosis and Survival in Hepatocellular Carcinoma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Rishabh Khatri, MD
Temple University Hospital
Philadelphia, Pennsylvania
Presenting Author(s)
Rishabh Khatri, MD1, Daohai Yu, PhD2, Frank Friedenberg, MD, MS2
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
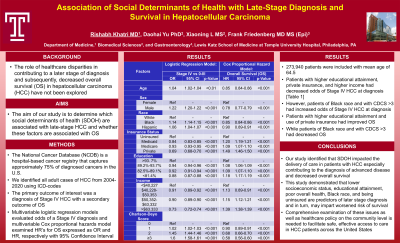
Introduction: The role of healthcare disparities in contributing to a later stage of diagnosis and decreased overall survival (OS) in hepatocellular carcinoma (HCC) has not been explored. Our study aimed to determine which social determinants of health (SDOH) are associated with late-stage HCC and whether these factors are associated with survival. We utilized the National Cancer Database (NCDB), a hospital-based cancer registry that captures approximately 75% of diagnosed cancers in the U.S. and Puerto Rico to explore this issue.
Methods: We identified all adult cases of HCC in the NCDB from 2004-2020. The primary outcome of interest was a diagnosis of Stage IV HCC with a secondary outcome of OS. Demographic cofactors included race, income, education via percent high school completion (HSC), insurance status and Charlson-Deyo comorbidity score (CDCS). Multivariable logistic regression models evaluated odds of a Stage IV diagnosis. Multivariable Cox proportional hazards model examined HR’s for OS. Analysis was performed using STATA.
Results: 273,940 patients were included with mean age of 64.5 (SD 11.1). In univariate analysis, higher education, income, and insurance status decreased the odds of Stage IV cancer at diagnosis, while Black race increased it. In multivariable analysis [Table 1], higher education [ >93.7% HSC vs < 81.4%, OR 0.88 (0.87-0.88)], private insurance [vs uninsured, OR 0.69 (0.68-0.70)] and higher income decreased the odds of Stage IV HCC diagnosis, whereas Black race [vs White OR 1.14 (1.14-1.15)] and CDCS ≥3 [vs 0, OR 1.60 (1.58-1.61)] increased the odds of Stage IV HCC. In the adjusted Cox proportional hazard model, higher education [ >93.7% HSC vs < 81.4%, HR 0.85 (0.85-0.86)], income >$63,333 [vs < $40,227, HR 0.72 (0.72-0.73)], private insurance [vs uninsured, HR 0.67 (0.67-0.69)] improved OS, whereas Black race [vs White HR 1.18 (1.18-1.19)] and CDCS ≥3 [vs 0, HR 1.71 (1.7-1.72)] decreased it.
Discussion: SDOH impacted the delivery of care in patients with HCC especially contributing to the diagnosis of advanced disease and decreased overall survival. This study demonstrated that lower socioeconomic status, educational attainment, poor overall health, Black race, and being uninsured are predictors of later stage diagnosis and in turn, may impart worsened risk of survival. Reducing disparities in cancer care require collective investment of healthcare providers, policymakers, and public health officials.
Disclosures:
Rishabh Khatri, MD1, Daohai Yu, PhD2, Frank Friedenberg, MD, MS2. P4096 - Association of Social Determinants of Health With Late-Stage Diagnosis and Survival in Hepatocellular Carcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: The role of healthcare disparities in contributing to a later stage of diagnosis and decreased overall survival (OS) in hepatocellular carcinoma (HCC) has not been explored. Our study aimed to determine which social determinants of health (SDOH) are associated with late-stage HCC and whether these factors are associated with survival. We utilized the National Cancer Database (NCDB), a hospital-based cancer registry that captures approximately 75% of diagnosed cancers in the U.S. and Puerto Rico to explore this issue.
Methods: We identified all adult cases of HCC in the NCDB from 2004-2020. The primary outcome of interest was a diagnosis of Stage IV HCC with a secondary outcome of OS. Demographic cofactors included race, income, education via percent high school completion (HSC), insurance status and Charlson-Deyo comorbidity score (CDCS). Multivariable logistic regression models evaluated odds of a Stage IV diagnosis. Multivariable Cox proportional hazards model examined HR’s for OS. Analysis was performed using STATA.
Results: 273,940 patients were included with mean age of 64.5 (SD 11.1). In univariate analysis, higher education, income, and insurance status decreased the odds of Stage IV cancer at diagnosis, while Black race increased it. In multivariable analysis [Table 1], higher education [ >93.7% HSC vs < 81.4%, OR 0.88 (0.87-0.88)], private insurance [vs uninsured, OR 0.69 (0.68-0.70)] and higher income decreased the odds of Stage IV HCC diagnosis, whereas Black race [vs White OR 1.14 (1.14-1.15)] and CDCS ≥3 [vs 0, OR 1.60 (1.58-1.61)] increased the odds of Stage IV HCC. In the adjusted Cox proportional hazard model, higher education [ >93.7% HSC vs < 81.4%, HR 0.85 (0.85-0.86)], income >$63,333 [vs < $40,227, HR 0.72 (0.72-0.73)], private insurance [vs uninsured, HR 0.67 (0.67-0.69)] improved OS, whereas Black race [vs White HR 1.18 (1.18-1.19)] and CDCS ≥3 [vs 0, HR 1.71 (1.7-1.72)] decreased it.
Discussion: SDOH impacted the delivery of care in patients with HCC especially contributing to the diagnosis of advanced disease and decreased overall survival. This study demonstrated that lower socioeconomic status, educational attainment, poor overall health, Black race, and being uninsured are predictors of later stage diagnosis and in turn, may impart worsened risk of survival. Reducing disparities in cancer care require collective investment of healthcare providers, policymakers, and public health officials.
Disclosures:
Rishabh Khatri indicated no relevant financial relationships.
Daohai Yu indicated no relevant financial relationships.
Frank Friedenberg indicated no relevant financial relationships.
Rishabh Khatri, MD1, Daohai Yu, PhD2, Frank Friedenberg, MD, MS2. P4096 - Association of Social Determinants of Health With Late-Stage Diagnosis and Survival in Hepatocellular Carcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
