Tuesday Poster Session
Category: Small Intestine
P4135 - Retroperitoneal Fibrosis Presenting With Upper Gastrointestinal Obstruction: A Very Rare Presentation of an Uncommon Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- JG
Jacob J. Gries, MD, MSc
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Jacob J.. Gries, MD, MSc1, Bing Chen, MD1, Bradley D. Confer, DO1, David L. Diehl, MD1, M. Amer swid, MD2
1Geisinger Medical Center, Danville, PA; 2Geisinger Medical center, Danville, PA
Introduction: Retroperitoneal fibrosis (RPF) is a rare chronic inflammatory disease causing fibrosis in the retroperitoneum which compresses adjacent structures, usually the ureters. It can be idiopathic (immunoglobin G4 (IgG4)- or non-IgG4-related) or secondary to various factors such as drugs, malignancy, infections, radiation therapy, and surgery1. Steroid therapy is effective in treating idiopathic RPF or as an adjunct in severe secondary RPF2,3. While upper GI tract involvement is extremely rare, with only a few case reports documenting its involvement4, it can occur when fibrous extension externally compresses the duodenum. We present a unique case of upper GI obstruction due to fibrous extension from the retroperitoneum that prompted workup and eventual diagnosis of RPF.
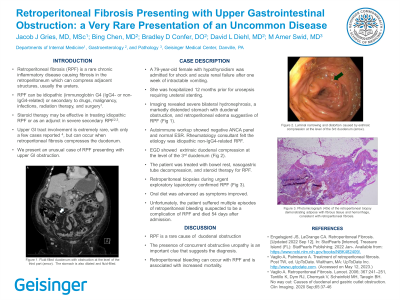
Case Description/Methods: The patient is a 79-year-old female with hypothyroidism admitted to the ICU for shock and acute renal failure after one week of intractable vomiting and constipation. She had a recent hospitalization several months prior for urosepsis requiring ureteral stenting, and another hospitalization one month prior for acute cholangitis requiring combination ERCP and laparoscopic cholecystectomy. Imaging revealed severe bilateral hydronephrosis, a markedly distended stomach with decompressed duodenum, and retroperitoneal edema suggestive of RPF (Figure 1). Autoimmune workup was noncontributory with negative ANCA panel and normal ESR. Rheumatology was consulted and determined the etiology to be idiopathic non-IgG4-related RPF; however, a suitable biopsy site was unable to be found by Interventional Radiology for tissue confirmation. EGD demonstrated extrinsic duodenal compression at the level of the 3rd duodenum (Figure 2). The patient was treated with bowel rest, nasogastric tube decompression, and steroid therapy for RPF. Oral diet was advanced as symptoms improved. Unfortunately, the patient suffered multiple episodes of retroperitoneal bleeding suspected to be a complication of RPF and died later in the admission. Tissue samples obtained during emergent exploratory laparotomy confirmed the presence of RPF (Figure 3).
Discussion: Prompt diagnosis and management are crucial to prevent complications of upper GI obstructions and improve patient outcomes. Our case highlights the importance of considering rare diseases such as RPF as a potential etiology for obstruction after intrinsic obstruction has been ruled out, especially in the presence of concurrent obstructive uropathy.

Disclosures:
Jacob J.. Gries, MD, MSc1, Bing Chen, MD1, Bradley D. Confer, DO1, David L. Diehl, MD1, M. Amer swid, MD2. P4135 - Retroperitoneal Fibrosis Presenting With Upper Gastrointestinal Obstruction: A Very Rare Presentation of an Uncommon Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisinger Medical center, Danville, PA
Introduction: Retroperitoneal fibrosis (RPF) is a rare chronic inflammatory disease causing fibrosis in the retroperitoneum which compresses adjacent structures, usually the ureters. It can be idiopathic (immunoglobin G4 (IgG4)- or non-IgG4-related) or secondary to various factors such as drugs, malignancy, infections, radiation therapy, and surgery1. Steroid therapy is effective in treating idiopathic RPF or as an adjunct in severe secondary RPF2,3. While upper GI tract involvement is extremely rare, with only a few case reports documenting its involvement4, it can occur when fibrous extension externally compresses the duodenum. We present a unique case of upper GI obstruction due to fibrous extension from the retroperitoneum that prompted workup and eventual diagnosis of RPF.
Case Description/Methods: The patient is a 79-year-old female with hypothyroidism admitted to the ICU for shock and acute renal failure after one week of intractable vomiting and constipation. She had a recent hospitalization several months prior for urosepsis requiring ureteral stenting, and another hospitalization one month prior for acute cholangitis requiring combination ERCP and laparoscopic cholecystectomy. Imaging revealed severe bilateral hydronephrosis, a markedly distended stomach with decompressed duodenum, and retroperitoneal edema suggestive of RPF (Figure 1). Autoimmune workup was noncontributory with negative ANCA panel and normal ESR. Rheumatology was consulted and determined the etiology to be idiopathic non-IgG4-related RPF; however, a suitable biopsy site was unable to be found by Interventional Radiology for tissue confirmation. EGD demonstrated extrinsic duodenal compression at the level of the 3rd duodenum (Figure 2). The patient was treated with bowel rest, nasogastric tube decompression, and steroid therapy for RPF. Oral diet was advanced as symptoms improved. Unfortunately, the patient suffered multiple episodes of retroperitoneal bleeding suspected to be a complication of RPF and died later in the admission. Tissue samples obtained during emergent exploratory laparotomy confirmed the presence of RPF (Figure 3).
Discussion: Prompt diagnosis and management are crucial to prevent complications of upper GI obstructions and improve patient outcomes. Our case highlights the importance of considering rare diseases such as RPF as a potential etiology for obstruction after intrinsic obstruction has been ruled out, especially in the presence of concurrent obstructive uropathy.

Figure: Figure 1. A) Fluid-filled duodenum measuring 3.5 cm with smooth muscle transition into the jejunum. B) Luminal narrowing and distortion caused by extrinsic compression at the level of the 3rd duodenum. C) Photomicrograph (100x) of the retroperitoneal biopsy demonstrating adipose with fibrous tissue and hemorrhage, consistent with retroperitoneal fibrosis.
Disclosures:
Jacob Gries indicated no relevant financial relationships.
Bing Chen indicated no relevant financial relationships.
Bradley Confer: Boston Scientific Corporation – Consultant.
David Diehl: Boston Scientific – Consultant. Castle – Consultant. Laborie – Consultant. Merit Endotek – Consultant. Microtech – Consultant. Olympus – Consultant. OnePass Medical – Consultant. Pentax – Consultant. Steris – Consultant.
M. Amer swid indicated no relevant financial relationships.
Jacob J.. Gries, MD, MSc1, Bing Chen, MD1, Bradley D. Confer, DO1, David L. Diehl, MD1, M. Amer swid, MD2. P4135 - Retroperitoneal Fibrosis Presenting With Upper Gastrointestinal Obstruction: A Very Rare Presentation of an Uncommon Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

