Tuesday Poster Session
Category: Stomach
P4186 - Managing Stress Ulcers in the ICU: What Medical Residents Know and Do
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Tolga Gidener, MD
SUNY Downstate
Brooklyn, New York
Presenting Author(s)
Tolga Gidener, MD1, Justin Chung, MD2, Qi Yu, MD, MPH3
1SUNY Downstate, Brooklyn, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3SUNY Downstate Health Sciences University/NYCHHC Kings County Hospital, Brooklyn, NY
Introduction: Critically ill patients in intensive care units (ICU) are at high risk of stress ulcers and ulcer-related bleeding. Proton pump inhibitors (PPIs) are commonly used to prevent acid production in the ICU setting, but there is a lack of clear guidelines regarding patient selection, intensity, timing, and de-escalation of therapy. This variability in practice influences how residents learn to prescribe PPIs for stress ulcer prophylaxis (SUP).
Methods: To address this issue, we conducted a survey of 184 internal medicine (IM) residents across three teaching hospitals to evaluate their knowledge, practices, and concerns regarding PPI use for SUP.
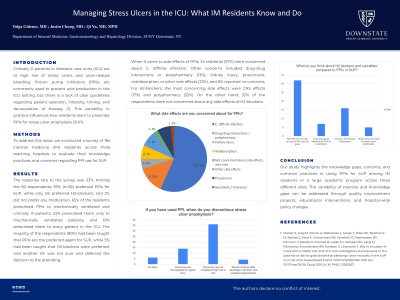
Results: The response rate to the survey was 33%. Among the 60 respondents, 93% (n=56) preferred PPIs for SUP, while only 5% preferred H2-blockers, and 2% did not prefer any medication. 65% of the residents prescribed PPIs to mechanically ventilated and critically ill patients, 22% prescribed them only to mechanically ventilated patients, and 10% prescribed them to every patient in the ICU. The majority of the respondents (90%) had been taught that PPIs are the preferred agent for SUP, while 5% had been taught that H2-blockers were preferred, and another 5% was not sure and deferred the decision to the attending.
When it came to side effects of PPIs, 34 residents (57%) were concerned about C. difficile infection. Other concerns included drug-drug interactions or polypharmacy (13%), kidney injury, pneumonia, malabsorption, or other side effects (22%), and 8% reported no concerns. For H2-blockers, the most concerning side effects were CNS effects (17%) and polypharmacy (32%). On the other hand, 32% of the respondents were not concerned about any side effects of H2-blockers. Regarding discontinuation of PPIs, 60% of the respondents reported that they discontinue PPIs once patients are not considered 'high risk' in the ICU, while 17% preferred to discontinue them after ICU downgrade, and 8% after discharge.
Discussion: Our study highlights the knowledge gaps, concerns, and common practices in using PPIs for SUP among IM residents in a large academic program across three different sites. The variability of practice and knowledge gaps can be addressed through quality improvement projects, educational interventions, and hospital-wide policy changes.

Disclosures:
Tolga Gidener, MD1, Justin Chung, MD2, Qi Yu, MD, MPH3. P4186 - Managing Stress Ulcers in the ICU: What Medical Residents Know and Do, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SUNY Downstate, Brooklyn, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3SUNY Downstate Health Sciences University/NYCHHC Kings County Hospital, Brooklyn, NY
Introduction: Critically ill patients in intensive care units (ICU) are at high risk of stress ulcers and ulcer-related bleeding. Proton pump inhibitors (PPIs) are commonly used to prevent acid production in the ICU setting, but there is a lack of clear guidelines regarding patient selection, intensity, timing, and de-escalation of therapy. This variability in practice influences how residents learn to prescribe PPIs for stress ulcer prophylaxis (SUP).
Methods: To address this issue, we conducted a survey of 184 internal medicine (IM) residents across three teaching hospitals to evaluate their knowledge, practices, and concerns regarding PPI use for SUP.
Results: The response rate to the survey was 33%. Among the 60 respondents, 93% (n=56) preferred PPIs for SUP, while only 5% preferred H2-blockers, and 2% did not prefer any medication. 65% of the residents prescribed PPIs to mechanically ventilated and critically ill patients, 22% prescribed them only to mechanically ventilated patients, and 10% prescribed them to every patient in the ICU. The majority of the respondents (90%) had been taught that PPIs are the preferred agent for SUP, while 5% had been taught that H2-blockers were preferred, and another 5% was not sure and deferred the decision to the attending.
When it came to side effects of PPIs, 34 residents (57%) were concerned about C. difficile infection. Other concerns included drug-drug interactions or polypharmacy (13%), kidney injury, pneumonia, malabsorption, or other side effects (22%), and 8% reported no concerns. For H2-blockers, the most concerning side effects were CNS effects (17%) and polypharmacy (32%). On the other hand, 32% of the respondents were not concerned about any side effects of H2-blockers. Regarding discontinuation of PPIs, 60% of the respondents reported that they discontinue PPIs once patients are not considered 'high risk' in the ICU, while 17% preferred to discontinue them after ICU downgrade, and 8% after discharge.
Discussion: Our study highlights the knowledge gaps, concerns, and common practices in using PPIs for SUP among IM residents in a large academic program across three different sites. The variability of practice and knowledge gaps can be addressed through quality improvement projects, educational interventions, and hospital-wide policy changes.

Figure: A- Medicine residents' practice in discontinuing PPI for stress ulcer prophylaxis in ICU
B- Medicine residents' thoughts on the side effect profile of PPIs
B- Medicine residents' thoughts on the side effect profile of PPIs
Disclosures:
Tolga Gidener indicated no relevant financial relationships.
Justin Chung indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Tolga Gidener, MD1, Justin Chung, MD2, Qi Yu, MD, MPH3. P4186 - Managing Stress Ulcers in the ICU: What Medical Residents Know and Do, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
