Tuesday Poster Session
Category: Stomach
P4191 - Mixed Adenoneuroendocrine Carcinoma of the Stomach: A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Reshad Salam, MD
Ascension Providence Hospital/Michigan State University
Southfield, Michigan
Presenting Author(s)
Reshad Salam, MD1, Eric Martin Sieloff, MD2, Michael Piper, MD3
1Ascension Providence Hospital/Michigan State University, Southfield, MI; 2Ascension Providence Southfield Hospital/ Michigan State University, Southfield, MI; 3Michigan State University/Ascension Providence - Providence Park Hospital, Southfield, MI
Introduction: Mixed adenoneuroendocrine carcinoma (MANEC) is a rare and poorly understood neoplasm of the gastrointestinal tract. It is characterized by the coexistence of adenocarcinoma and neuroendocrine carcinoma components. MANECs have a poor prognosis due to the malignant nature of both components. Gastric MANEC (gMANEC) is particularly rare, with limited epidemiological data available, making it difficult to establish effective treatment strategies. We present a case of a gastric MANEC and provide a review of the existing literature on this rare tumor type, highlighting the need for early diagnosis and improved understanding of its pathogenesis.
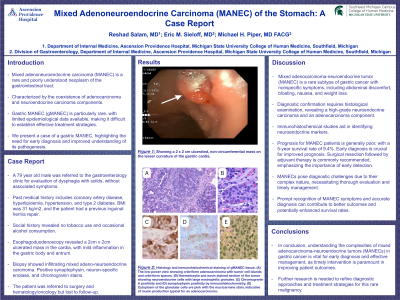
Case Description/Methods: A 79 year old male was referred to the gastroenterology clinic for evaluation of dysphagia for solids, without associated symptoms. Past medical history includes coronary artery disease, hyperlipidemia, hypertension, and type 2 diabetes. BMI was 31 kg/m2, and the patient had a previous inguinal hernia repair. Social history revealed no tobacco use and occasional alcohol consumption. Esophagoduodenoscopy revealed a 2cm x 2cm ulcerated mass in the cardia, with mild inflammation in the gastric body and antrum. Biopsy showed infiltrating mixed adenocarcinoma-neuroendocrine carcinoma. Positive synaptophysin, neuron-specific enolase, and chromogranin stains. The patient was referred to surgery and hematology/oncology but lost to follow-up.
Discussion: Mixed adenocarcinoma-neuroendocrine tumor (MANEC) is a rare subtype of gastric cancer with nonspecific symptoms, including abdominal discomfort, bloating, nausea, and weight loss. Early diagnosis is crucial for improved prognosis. Diagnostic confirmation requires histological examination, revealing a high-grade neuroendocrine carcinoma and an adenocarcinoma component. Immunohistochemical studies aid in identifying neuroendocrine markers. Prognosis for MANEC patients is generally poor, with a 5-year survival rate of 9.4%. Surgical resection followed by adjuvant therapy is commonly recommended, emphasizing the importance of early detection. MANECs pose diagnostic challenges due to their complex nature, necessitating thorough evaluation and timely management. Prompt recognition of MANEC symptoms and accurate diagnosis can contribute to better outcomes and potentially enhanced survival rates.

Disclosures:
Reshad Salam, MD1, Eric Martin Sieloff, MD2, Michael Piper, MD3. P4191 - Mixed Adenoneuroendocrine Carcinoma of the Stomach: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Ascension Providence Hospital/Michigan State University, Southfield, MI; 2Ascension Providence Southfield Hospital/ Michigan State University, Southfield, MI; 3Michigan State University/Ascension Providence - Providence Park Hospital, Southfield, MI
Introduction: Mixed adenoneuroendocrine carcinoma (MANEC) is a rare and poorly understood neoplasm of the gastrointestinal tract. It is characterized by the coexistence of adenocarcinoma and neuroendocrine carcinoma components. MANECs have a poor prognosis due to the malignant nature of both components. Gastric MANEC (gMANEC) is particularly rare, with limited epidemiological data available, making it difficult to establish effective treatment strategies. We present a case of a gastric MANEC and provide a review of the existing literature on this rare tumor type, highlighting the need for early diagnosis and improved understanding of its pathogenesis.
Case Description/Methods: A 79 year old male was referred to the gastroenterology clinic for evaluation of dysphagia for solids, without associated symptoms. Past medical history includes coronary artery disease, hyperlipidemia, hypertension, and type 2 diabetes. BMI was 31 kg/m2, and the patient had a previous inguinal hernia repair. Social history revealed no tobacco use and occasional alcohol consumption. Esophagoduodenoscopy revealed a 2cm x 2cm ulcerated mass in the cardia, with mild inflammation in the gastric body and antrum. Biopsy showed infiltrating mixed adenocarcinoma-neuroendocrine carcinoma. Positive synaptophysin, neuron-specific enolase, and chromogranin stains. The patient was referred to surgery and hematology/oncology but lost to follow-up.
Discussion: Mixed adenocarcinoma-neuroendocrine tumor (MANEC) is a rare subtype of gastric cancer with nonspecific symptoms, including abdominal discomfort, bloating, nausea, and weight loss. Early diagnosis is crucial for improved prognosis. Diagnostic confirmation requires histological examination, revealing a high-grade neuroendocrine carcinoma and an adenocarcinoma component. Immunohistochemical studies aid in identifying neuroendocrine markers. Prognosis for MANEC patients is generally poor, with a 5-year survival rate of 9.4%. Surgical resection followed by adjuvant therapy is commonly recommended, emphasizing the importance of early detection. MANECs pose diagnostic challenges due to their complex nature, necessitating thorough evaluation and timely management. Prompt recognition of MANEC symptoms and accurate diagnosis can contribute to better outcomes and potentially enhanced survival rates.

Figure: Figure 2: Histology and immunohistochemical staining of gMENAC tissue. (A) The low-power view showing cribriform adenocarcinoma with tumor cell islands and cribriform spaces. (B) Haematoxylin and eosin stained section of the tumor showing neuroendocrine cells with large eosinophilic granules. (C) Chromogranin A positivity and (D) synaptophysin positivity by immunohistochemistry. (E) Cytoplasm of the glandular cells are pink with the mucicarmine stain, indicative of mucin production typical for an adenocarcinoma.
Disclosures:
Reshad Salam indicated no relevant financial relationships.
Eric Martin Sieloff indicated no relevant financial relationships.
Michael Piper indicated no relevant financial relationships.
Reshad Salam, MD1, Eric Martin Sieloff, MD2, Michael Piper, MD3. P4191 - Mixed Adenoneuroendocrine Carcinoma of the Stomach: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
