Tuesday Poster Session
Category: Stomach
P4192 - Composite Mesh in Incisional Hernia Repair: A Case Report of Unprecedented Gastric Penetration and Gastrocutaneous Fistula Formation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Mohammad AbuAssi, MD
University of Central Florida College of Medicine
Gainesville, FL
Presenting Author(s)
Award: Presidential Poster Award
Mohammad Abuassi, MD1, Diala Burjak, MS2, Husam Shakour, MD2, Somtochukwu Onwuzo, MD3, Antoine Boustany, MD, MPH4, Aon Ryalat, MD2, Aiman Obed, MD, PhD2
1University of Central Florida College of Medicine, Gainesville, FL; 2Jordan Hospital, Amman, 'Amman, Jordan; 3Cleveland Clinic Foundation, Fairview Park, OH; 4Cleveland Clinic Foundation, Cleveland, OH
Introduction: Hernia repair frequently employs surgical mesh, reducing recurrence rates substantially. However, potential complications exist, including infection, chronic pain, and mesh migration and erosion into adjacent organs, leading to serious outcomes such as enteric fistulas. We report an unprecedented case of composite mesh leading to gastric penetration and subsequent gastrocutaneous fistula formation, identified during endoscopic investigation as a foreign body.
Case Description/Methods: A 70-year-old male with a history of atrial fibrillation and colon cancer, who underwent right hemicolectomy in 2008 and incisional hernia repair using composite mesh in 2010, presented in June 2022 with symptoms of intestinal obstruction and a small bowel content leak. Following these complications, a small bowel resection was performed, and an ileostomy was created. By March 2023, the patient developed an enterocutaneous fistula. During an endoscopic investigation, the composite mesh used in the previous hernia repair was found as a foreign body penetrating the gastric antral area, causing a gastrocutaneous fistula. An exploratory laparotomy was successfully carried out, the mesh was removed, and the gastric perforation was surgically repaired. The patient's recovery was uneventful, with no further complications.
Discussion: Though mesh erosion into the gastrointestinal tract is a rare yet known complication, we report a novel finding of mesh erosion leading to gastric penetration. The unique properties of composite mesh, which promotes tissue ingrowth and minimizes visceral adhesions, combined with individual patient factors and surgical technique specifics, likely contributed to this atypical complication.
Managing mesh-related gastrointestinal complications can be intricate and necessitates a multidisciplinary approach. In our case, the mesh causing the gastric fistula was successfully removed, and the resultant gastric perforation was surgically repaired. Despite the use of conservative approaches such as vacuum dressing and Total Parenteral Nutrition (TPN), the abdominal wall fistula remained unresponsive.
The case underscores the need for vigilance towards mesh-related complications in patients with unanticipated post-operative symptoms post-incisional hernia repair. It signals an exigency for further research to understand factors contributing to mesh erosion and fistula formation and to devise strategies for preventing such complications.

Disclosures:
Mohammad Abuassi, MD1, Diala Burjak, MS2, Husam Shakour, MD2, Somtochukwu Onwuzo, MD3, Antoine Boustany, MD, MPH4, Aon Ryalat, MD2, Aiman Obed, MD, PhD2. P4192 - Composite Mesh in Incisional Hernia Repair: A Case Report of Unprecedented Gastric Penetration and Gastrocutaneous Fistula Formation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mohammad Abuassi, MD1, Diala Burjak, MS2, Husam Shakour, MD2, Somtochukwu Onwuzo, MD3, Antoine Boustany, MD, MPH4, Aon Ryalat, MD2, Aiman Obed, MD, PhD2
1University of Central Florida College of Medicine, Gainesville, FL; 2Jordan Hospital, Amman, 'Amman, Jordan; 3Cleveland Clinic Foundation, Fairview Park, OH; 4Cleveland Clinic Foundation, Cleveland, OH
Introduction: Hernia repair frequently employs surgical mesh, reducing recurrence rates substantially. However, potential complications exist, including infection, chronic pain, and mesh migration and erosion into adjacent organs, leading to serious outcomes such as enteric fistulas. We report an unprecedented case of composite mesh leading to gastric penetration and subsequent gastrocutaneous fistula formation, identified during endoscopic investigation as a foreign body.
Case Description/Methods: A 70-year-old male with a history of atrial fibrillation and colon cancer, who underwent right hemicolectomy in 2008 and incisional hernia repair using composite mesh in 2010, presented in June 2022 with symptoms of intestinal obstruction and a small bowel content leak. Following these complications, a small bowel resection was performed, and an ileostomy was created. By March 2023, the patient developed an enterocutaneous fistula. During an endoscopic investigation, the composite mesh used in the previous hernia repair was found as a foreign body penetrating the gastric antral area, causing a gastrocutaneous fistula. An exploratory laparotomy was successfully carried out, the mesh was removed, and the gastric perforation was surgically repaired. The patient's recovery was uneventful, with no further complications.
Discussion: Though mesh erosion into the gastrointestinal tract is a rare yet known complication, we report a novel finding of mesh erosion leading to gastric penetration. The unique properties of composite mesh, which promotes tissue ingrowth and minimizes visceral adhesions, combined with individual patient factors and surgical technique specifics, likely contributed to this atypical complication.
Managing mesh-related gastrointestinal complications can be intricate and necessitates a multidisciplinary approach. In our case, the mesh causing the gastric fistula was successfully removed, and the resultant gastric perforation was surgically repaired. Despite the use of conservative approaches such as vacuum dressing and Total Parenteral Nutrition (TPN), the abdominal wall fistula remained unresponsive.
The case underscores the need for vigilance towards mesh-related complications in patients with unanticipated post-operative symptoms post-incisional hernia repair. It signals an exigency for further research to understand factors contributing to mesh erosion and fistula formation and to devise strategies for preventing such complications.

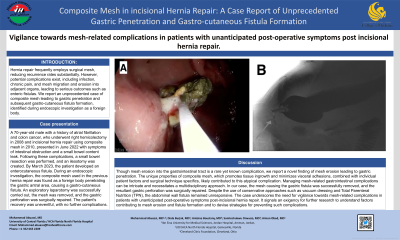
Figure: Panel A: Endoscopic view reveals a foreign body infiltrating the gastric antral area. Panel B: Gastrografin barium meal distinctly visualizes an anomalous passage connecting the anterior portion of the gastric antrum with the subcutaneous tissue of the abdominal wall.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Diala Burjak indicated no relevant financial relationships.
Husam Shakour indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Aon Ryalat indicated no relevant financial relationships.
Aiman Obed indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Diala Burjak, MS2, Husam Shakour, MD2, Somtochukwu Onwuzo, MD3, Antoine Boustany, MD, MPH4, Aon Ryalat, MD2, Aiman Obed, MD, PhD2. P4192 - Composite Mesh in Incisional Hernia Repair: A Case Report of Unprecedented Gastric Penetration and Gastrocutaneous Fistula Formation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

