Tuesday Poster Session
Category: Stomach
P4237 - Buried Balloon Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Porsha Okiye, MD
Augusta University Medical Center
Augusta, GA
Presenting Author(s)
Porsha Okiye, MD1, Amit R. Hudgi, MBBS1, Praneeth Kudaravalli, MD2, Humberto Sifuentes, MD2
1Augusta University Medical Center, Augusta, GA; 2Augusta University, Augusta, GA
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are the hallmark of management to optimize long-term enteral nutrition for individuals with inadequate oral intake. Despite the advantage of safe enteral access, complications including buried bumper syndrome (BBS) are well recognized. BBS occurs when the internal fixation device migrates along the stoma tract between the stomach and the overlying skin causing erosion. BBS is typically observed in PEG devices with rigid or small contact area due to increased risk of pressure necrosis of the gastric mucosai. Balloon PEG tube has a smaller internal bumper, thus reduced risk for this complication. We report a rare complication of buried bumper syndrome associated with balloon gastrostomy tube.
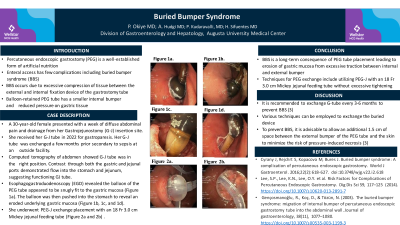
Case Description/Methods: A 30 year old female with history of uncontrolled type I diabetes mellitus presented with a week of abdominal pain, nausea, vomiting, and drainage from her Gastrojejunostomy (G-J) insertion site. She received her G-J tube in 2022 for gastroparesis. She reported her G-J tube was exchanged a few months prior due to sepsis at an outside facility. On exam, there was serous drainage at G-J tube site with tenderness. Lab results were significant for normocytic anemia, however white blood cell count, liver enzymes, and lipase were unremarkable. Computed tomography of abdomen showed G-J tube was in the appropriate position. Contrast injection through the gastric and jejunal ports demonstrated flow into the stomach and jejunum respectively, suggesting properly functioning GJ tube. Esophagogastroduodenoscopy (EGD) revealed the balloon PEG tube snugly fit to the gastric mucosa (Figure 1a). The balloon was then pushed into the stomach to reveal an eroded underlying gastric mucosa (Figure 1b, c, and d). The patient was placed on a clear liquid diet and Proton Pump Inhibitor (PPI) was initiated with erythromycin to facilitate peristalsis of gastric contents. She underwent PEG-J exchange placement with an 18 Fr 3.0 cm Mickey jejunal feeding tube. Patient’s tube feeds were resumed without complications.
Discussion: BBS is a well identified rare consequence of PEG tube placement leading to erosion of gastric mucosa secondary to tension between the internal and external bumpers of the G-tube. Is it recommended to exchange G-tube every 3-6 months to prevent BBS. Many techniques have been described for PEG exchange. In this case, a PEG-J with an 18 Fr 3.0 cm Mickey jejunal feeding tube, without recurrence of BBS.

Disclosures:
Porsha Okiye, MD1, Amit R. Hudgi, MBBS1, Praneeth Kudaravalli, MD2, Humberto Sifuentes, MD2. P4237 - Buried Balloon Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Augusta University Medical Center, Augusta, GA; 2Augusta University, Augusta, GA
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are the hallmark of management to optimize long-term enteral nutrition for individuals with inadequate oral intake. Despite the advantage of safe enteral access, complications including buried bumper syndrome (BBS) are well recognized. BBS occurs when the internal fixation device migrates along the stoma tract between the stomach and the overlying skin causing erosion. BBS is typically observed in PEG devices with rigid or small contact area due to increased risk of pressure necrosis of the gastric mucosai. Balloon PEG tube has a smaller internal bumper, thus reduced risk for this complication. We report a rare complication of buried bumper syndrome associated with balloon gastrostomy tube.
Case Description/Methods: A 30 year old female with history of uncontrolled type I diabetes mellitus presented with a week of abdominal pain, nausea, vomiting, and drainage from her Gastrojejunostomy (G-J) insertion site. She received her G-J tube in 2022 for gastroparesis. She reported her G-J tube was exchanged a few months prior due to sepsis at an outside facility. On exam, there was serous drainage at G-J tube site with tenderness. Lab results were significant for normocytic anemia, however white blood cell count, liver enzymes, and lipase were unremarkable. Computed tomography of abdomen showed G-J tube was in the appropriate position. Contrast injection through the gastric and jejunal ports demonstrated flow into the stomach and jejunum respectively, suggesting properly functioning GJ tube. Esophagogastroduodenoscopy (EGD) revealed the balloon PEG tube snugly fit to the gastric mucosa (Figure 1a). The balloon was then pushed into the stomach to reveal an eroded underlying gastric mucosa (Figure 1b, c, and d). The patient was placed on a clear liquid diet and Proton Pump Inhibitor (PPI) was initiated with erythromycin to facilitate peristalsis of gastric contents. She underwent PEG-J exchange placement with an 18 Fr 3.0 cm Mickey jejunal feeding tube. Patient’s tube feeds were resumed without complications.
Discussion: BBS is a well identified rare consequence of PEG tube placement leading to erosion of gastric mucosa secondary to tension between the internal and external bumpers of the G-tube. Is it recommended to exchange G-tube every 3-6 months to prevent BBS. Many techniques have been described for PEG exchange. In this case, a PEG-J with an 18 Fr 3.0 cm Mickey jejunal feeding tube, without recurrence of BBS.

Figure: Figure 1a. Depicted is the balloon snuggly fitting in the gastric mucosa. Figures 1b,1c, and 1d are images used to depict the eroded gastric mucosa once the balloon was removed.
Disclosures:
Porsha Okiye indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Praneeth Kudaravalli indicated no relevant financial relationships.
Humberto Sifuentes indicated no relevant financial relationships.
Porsha Okiye, MD1, Amit R. Hudgi, MBBS1, Praneeth Kudaravalli, MD2, Humberto Sifuentes, MD2. P4237 - Buried Balloon Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
