Tuesday Poster Session
Category: Esophagus
P3294 - A Case of Successful Novel Dupilumab Use for Gastrointestinal Involvement of Idiopathic Hypereosinophilic Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- CS
Christopher Soriano, MD
UCLA
Los Angeles, CA
Presenting Author(s)
Christopher Soriano, MD1, Clare Moffatt, BSc2, Guy A. Weiss, MD2, David Dawson, MD1
1UCLA, Los Angeles, CA; 2University of California Los Angeles, Los Angeles, CA
Introduction: Hypereosinophilic syndrome (HES) is a rare, multisystem group of disorders characterized by tissue hypereosinophilia or persistent elevated eosinophil counts, with associated eosinophil-mediated organ damage. Gastrointestinal (GI) involvement is the third most common clinical manifestation. First-line treatment is systemic steroids. We present a patient with idiopathic HES with secondary eosinophilic esophagitis (EoE), eosinophilic gastritis (EoG), and eosinophilic enteritis (EoN), corticosteroids-dependent, azathioprine and mepolizumab-refractory. The patient achieved clinical and histopathologic remission following dupilumab treatment.
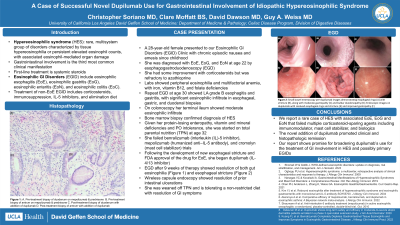
Case Description/Methods: A 28-year-old female presented to our Eosinophilic GI Disorders (EGID) Clinic with chronic episodic nausea and emesis since childhood. She was diagnosed with EGID at age 22 by esophagogastroduodenoscopy (EGD). She had some improvement with corticosteroids but was refractory to azathioprine. She was found to have peripheral eosinophilia and multifactorial anemia, with iron, vitamin B12, and folate deficiencies. Repeat EGD at age 30 showed LA grade B esophagitis and gastritis, with significant eosinophilic infiltrate in esophageal, gastric, and duodenal biopsies. On colonoscopy her terminal ileum showed moderate eosinophilic infiltrate. Bone marrow biopsy confirmed diagnosis of HES. Given her protein-losing enteropathy, vitamin and mineral deficiencies and PO intolerance, she was started on total parental nutrition (TPN) at age 32. She failed benralizumab (interleukin (IL)-5 inhibitor), mepolizumab (humanized anti–IL-5 antibody), and cromolyn (mast cell stabilizer) trials. Following the development of new esophageal stricture and FDA approval of the drug for EoE, she began dupilumab (IL-4/13 inhibitor) and after 9 weeks of therapy, EGD showed resolution of both esophageal stricture (Figure 1) and gut eosinophilia (Figure 2), and wireless capsule endoscopy showed resolution of prior intestinal ulcerations. She was weaned off TPN and is tolerating a non-restricted diet with resolution of GI symptoms.
Discussion: We report a rare case of HES with associated EoE, EoG and EoN that failed multiple corticosteroid-sparing agents including immunomodulator, mast cell stabilizer, and biologics. The novel addition of dupilumab promoted clinical and histopathologic remission. Our report shows promise for broadening dupilumab’s use for the treatment of GI involvement in HES and possibly primary EGIDs.

Disclosures:
Christopher Soriano, MD1, Clare Moffatt, BSc2, Guy A. Weiss, MD2, David Dawson, MD1. P3294 - A Case of Successful Novel Dupilumab Use for Gastrointestinal Involvement of Idiopathic Hypereosinophilic Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UCLA, Los Angeles, CA; 2University of California Los Angeles, Los Angeles, CA
Introduction: Hypereosinophilic syndrome (HES) is a rare, multisystem group of disorders characterized by tissue hypereosinophilia or persistent elevated eosinophil counts, with associated eosinophil-mediated organ damage. Gastrointestinal (GI) involvement is the third most common clinical manifestation. First-line treatment is systemic steroids. We present a patient with idiopathic HES with secondary eosinophilic esophagitis (EoE), eosinophilic gastritis (EoG), and eosinophilic enteritis (EoN), corticosteroids-dependent, azathioprine and mepolizumab-refractory. The patient achieved clinical and histopathologic remission following dupilumab treatment.
Case Description/Methods: A 28-year-old female presented to our Eosinophilic GI Disorders (EGID) Clinic with chronic episodic nausea and emesis since childhood. She was diagnosed with EGID at age 22 by esophagogastroduodenoscopy (EGD). She had some improvement with corticosteroids but was refractory to azathioprine. She was found to have peripheral eosinophilia and multifactorial anemia, with iron, vitamin B12, and folate deficiencies. Repeat EGD at age 30 showed LA grade B esophagitis and gastritis, with significant eosinophilic infiltrate in esophageal, gastric, and duodenal biopsies. On colonoscopy her terminal ileum showed moderate eosinophilic infiltrate. Bone marrow biopsy confirmed diagnosis of HES. Given her protein-losing enteropathy, vitamin and mineral deficiencies and PO intolerance, she was started on total parental nutrition (TPN) at age 32. She failed benralizumab (interleukin (IL)-5 inhibitor), mepolizumab (humanized anti–IL-5 antibody), and cromolyn (mast cell stabilizer) trials. Following the development of new esophageal stricture and FDA approval of the drug for EoE, she began dupilumab (IL-4/13 inhibitor) and after 9 weeks of therapy, EGD showed resolution of both esophageal stricture (Figure 1) and gut eosinophilia (Figure 2), and wireless capsule endoscopy showed resolution of prior intestinal ulcerations. She was weaned off TPN and is tolerating a non-restricted diet with resolution of GI symptoms.
Discussion: We report a rare case of HES with associated EoE, EoG and EoN that failed multiple corticosteroid-sparing agents including immunomodulator, mast cell stabilizer, and biologics. The novel addition of dupilumab promoted clinical and histopathologic remission. Our report shows promise for broadening dupilumab’s use for the treatment of GI involvement in HES and possibly primary EGIDs.

Figure: Figure 1. Small bowel enteroscopy pre-dupilumab images demonstrating esophageal rings (A) with stricture (B), along with moderate gastropathy (C) and bulbar duodenopathy (D) and Endoscopic images on dupilumab with resolved esophageal rings and stricture (E) and improved gastropathy (F).
Figure 2. Representative histologic images of pre-treatment biopsies from the duodenum (A) and gastric antrum (B) showing increased eosinophils within lamina propria, including degranulating forms and patchy infiltration of crypt and surface epithelium by eosinophils. In contrast, a reduction in eosinophils was observed in post-treatment biopsies from the duodenum (C) and gastric antrum (D).
Figure 2. Representative histologic images of pre-treatment biopsies from the duodenum (A) and gastric antrum (B) showing increased eosinophils within lamina propria, including degranulating forms and patchy infiltration of crypt and surface epithelium by eosinophils. In contrast, a reduction in eosinophils was observed in post-treatment biopsies from the duodenum (C) and gastric antrum (D).
Disclosures:
Christopher Soriano indicated no relevant financial relationships.
Clare Moffatt indicated no relevant financial relationships.
Guy Weiss: Everlywell – Advisory Committee/Board Member. Guidepoint – Consultant.
David Dawson indicated no relevant financial relationships.
Christopher Soriano, MD1, Clare Moffatt, BSc2, Guy A. Weiss, MD2, David Dawson, MD1. P3294 - A Case of Successful Novel Dupilumab Use for Gastrointestinal Involvement of Idiopathic Hypereosinophilic Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
