Tuesday Poster Session
Category: Esophagus
P3302 - Gastroesophageal Intussusception Treated Through cTIF in a Patient With Systemic Sclerosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Areeka Memon, DO, MPH
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Areeka Memon, DO, MPH1, Monique Hinchcliff, MD, MS2, Nicholas Dugan, MD3, Amir Masoud, MD4
1University of Connecticut Health, Farmington, CT; 2Yale School of Medicine, New Haven, CT; 3Hartford Healthcare, Hartford, CT; 4Neurogastroenterology and Motility Center, Hartford Healthcare, Connecticut GI PC, Hartford, CT
Introduction: Systemic sclerosis (SSc) is a rheumatic disease with the highest case-fatality rate whose pathogenesis involves autoimmunity and fibrosis. 50 to 90% of SSc patients experience GI symptoms, and GI involvement is the underlying cause of death in up to 12% of patients. Gastroesophageal (GE) intussusception is the invagination of the stomach into the esophagus and is mostly reported in felines and canines. Here, we present the first reported case of an SSc patient with hiatal hernia and GE intussusception who was successfully treated with concomitant hiatal hernia repair and transoral incisionless fundoplication (cTIF).
Case Description/Methods: A 49-year-old woman with a history of psoriasis, Raynaud phenomenon, polymyositis, interstitial lung disease, and diffuse cutaneous SSc was referred to gastroenterology for persistent pill dysphagia and progressive GE reflux despite pharmacologic treatment. The physical exam was noteworthy for microstomia, facial telangiectasia, sclerodactyly complicated by digital contractures of multiple interphalangeal (PIP) joints, classic for SSc. Laboratory studies revealed 1:320 anti-nuclear antibodies with a speckled pattern and CBC and CMP were within normal limits.
She underwent an esophagogastroduodenoscopy (EGD) which revealed an obstructing mass-like structure at the GE junction concerning for gastric intussusception, overlaying gastric polyp, and hiatal hernia (Image A). The gastric polyp was initially thought to be a lead point, and the patient underwent endoscopic mucosal resection and stenting (Image B). Unfortunately, she was unable to tolerate the stent due to intractable pain, and it was subsequently removed. Due to persistent reflux and dysphagia the patient underwent cTIF (Image C). Post-intervention dysphagia resolved, and reflux improved. She reported a mild decrease in ability to belch and some bloating after a follow-up period of six weeks.
Discussion: GE intussusception is an exceptionally rare phenomenon that occurred in the setting of SSc-related esophageal dilation and hiatal hernia. Symptoms can be refractory despite maximal medical therapy. SSc is a relative contraindication for laparoscopic fundoplication and a roux-en-y procedure has become the suggested standard of care for refractory GI symptoms in SSc patients. However, we demonstrate successful cTIF with near-complete resolution of GI symptoms.

Disclosures:
Areeka Memon, DO, MPH1, Monique Hinchcliff, MD, MS2, Nicholas Dugan, MD3, Amir Masoud, MD4. P3302 - Gastroesophageal Intussusception Treated Through cTIF in a Patient With Systemic Sclerosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2Yale School of Medicine, New Haven, CT; 3Hartford Healthcare, Hartford, CT; 4Neurogastroenterology and Motility Center, Hartford Healthcare, Connecticut GI PC, Hartford, CT
Introduction: Systemic sclerosis (SSc) is a rheumatic disease with the highest case-fatality rate whose pathogenesis involves autoimmunity and fibrosis. 50 to 90% of SSc patients experience GI symptoms, and GI involvement is the underlying cause of death in up to 12% of patients. Gastroesophageal (GE) intussusception is the invagination of the stomach into the esophagus and is mostly reported in felines and canines. Here, we present the first reported case of an SSc patient with hiatal hernia and GE intussusception who was successfully treated with concomitant hiatal hernia repair and transoral incisionless fundoplication (cTIF).
Case Description/Methods: A 49-year-old woman with a history of psoriasis, Raynaud phenomenon, polymyositis, interstitial lung disease, and diffuse cutaneous SSc was referred to gastroenterology for persistent pill dysphagia and progressive GE reflux despite pharmacologic treatment. The physical exam was noteworthy for microstomia, facial telangiectasia, sclerodactyly complicated by digital contractures of multiple interphalangeal (PIP) joints, classic for SSc. Laboratory studies revealed 1:320 anti-nuclear antibodies with a speckled pattern and CBC and CMP were within normal limits.
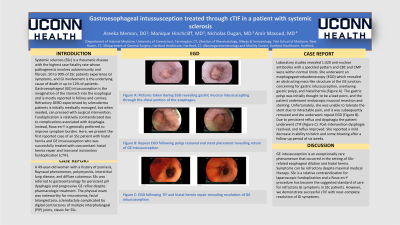
She underwent an esophagogastroduodenoscopy (EGD) which revealed an obstructing mass-like structure at the GE junction concerning for gastric intussusception, overlaying gastric polyp, and hiatal hernia (Image A). The gastric polyp was initially thought to be a lead point, and the patient underwent endoscopic mucosal resection and stenting (Image B). Unfortunately, she was unable to tolerate the stent due to intractable pain, and it was subsequently removed. Due to persistent reflux and dysphagia the patient underwent cTIF (Image C). Post-intervention dysphagia resolved, and reflux improved. She reported a mild decrease in ability to belch and some bloating after a follow-up period of six weeks.
Discussion: GE intussusception is an exceptionally rare phenomenon that occurred in the setting of SSc-related esophageal dilation and hiatal hernia. Symptoms can be refractory despite maximal medical therapy. SSc is a relative contraindication for laparoscopic fundoplication and a roux-en-y procedure has become the suggested standard of care for refractory GI symptoms in SSc patients. However, we demonstrate successful cTIF with near-complete resolution of GI symptoms.

Figure: Figure A: Picture taken during EGD revealing gastric mucosa intussuscepting through the distal portion of the esophagus.
Figure B: Repeat EGD following polyp removal and stent placement revealing return of GE intussusception.
Figure C: EGD following TIF and hiatal hernia repair revealing resolution of GE intussusception.
Figure B: Repeat EGD following polyp removal and stent placement revealing return of GE intussusception.
Figure C: EGD following TIF and hiatal hernia repair revealing resolution of GE intussusception.
Disclosures:
Areeka Memon indicated no relevant financial relationships.
Monique Hinchcliff: Boehringer Ingelheim – Grant/Research Support. Kadmon Pharmaceutical – Grant/Research Support.
Nicholas Dugan indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Areeka Memon, DO, MPH1, Monique Hinchcliff, MD, MS2, Nicholas Dugan, MD3, Amir Masoud, MD4. P3302 - Gastroesophageal Intussusception Treated Through cTIF in a Patient With Systemic Sclerosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
