Tuesday Poster Session
Category: Esophagus
P3309 - Esophageal Duplication Cysts: Diagnostic Challenges and Risk-Mitigating Approaches
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Abu Abbasi, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Abu Fahad Abbasi, MD1, Fnu Vikash, MD2, Joshua Almaraj, MD3, Filippa Trikantzopoulou, MD4, Promila Banerjee, MD1
1Loyola University Medical Center, Maywood, IL; 2Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 3Ross University, Maywood, IL; 4Loyola University Medical Center, Chicago, IL
Introduction: Esophageal duplication cysts (EDC) are rare congenital anomalies primarily occurring in embryonic development with 70% discovered in the 1st year of life. EDC requires three criteria: the cyst wall and gastric wall are contiguous, the cyst is surrounded by smooth muscle, and lined with gastric epithelium. Endoscopic ultrasonography (EUS) is the most common method for diagnosis. Anechogenic lesions are monitored conservatively whereas hypoechogenic lesions may require endoscopic ultrasound with fine needle aspiration (EUS-FNA). Symptomatic duplication cysts tend to require surgical management. EUS-FNA has a higher infection rate; however, effectively rules out deceiving malignant lesions. There is controversy within the literature regarding whether to complete FNA to confirm duplication cyst. Our case series emphasizes taking risk-migrating steps to decrease infections and determine a diagnosis.
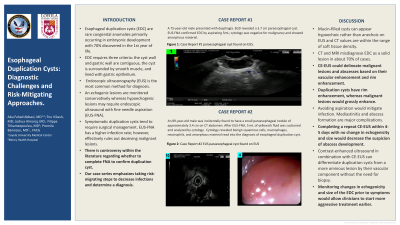
Case Description/Methods: An 89-year-old male was incidentally found to have a small paraesophageal nodule of approximately 3.4 cm on CT abdomen. After EUS-FNA, 5 mL of yellowish fluid was suctioned and analyzed by cytology. Cytology revealed benign squamous cells, macrophages, neutrophils, and amorphous material read into the diagnosis of esophageal duplication cyst.
A 75-year-old male presented with dysphagia. EGD revealed a 3.7 cm paraesophageal cyst. EUS-FNA confirmed EDC by aspirating 5mL; cytology was negative for malignancy and showed amorphous material.
Discussion: Mucin-filled cysts can appear hypoechoic rather than anechoic on EUS and CT values are within the range of soft tissue density. CT and MRI misdiagnose EDC as a solid lesion in about 70% of cases. CE-EUS could delineate malignant lesions and abscesses based on their vascular enhancement and rim enhancement. Duplication cysts have rim enhancement, whereas malignant lesions would grossly enhance. Avoiding aspiration would mitigate infection. Mediastinitis and abscess formation are major complications. Completing a repeat CE-EUS within 4-5 days with no change in echogenicity and size would decrease the suspicion of abscess development. Contrast-enhanced ultrasound in combination with endoscopic ultrasound (CE-EUS) can differentiate duplication cysts from a more ominous lesion by their vascular component without the need for biopsy. Monitoring changes in echogenicity and size of the EDC prior to symptoms would allow clinicians to start more aggressive treatment earlier.

Disclosures:
Abu Fahad Abbasi, MD1, Fnu Vikash, MD2, Joshua Almaraj, MD3, Filippa Trikantzopoulou, MD4, Promila Banerjee, MD1. P3309 - Esophageal Duplication Cysts: Diagnostic Challenges and Risk-Mitigating Approaches, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 3Ross University, Maywood, IL; 4Loyola University Medical Center, Chicago, IL
Introduction: Esophageal duplication cysts (EDC) are rare congenital anomalies primarily occurring in embryonic development with 70% discovered in the 1st year of life. EDC requires three criteria: the cyst wall and gastric wall are contiguous, the cyst is surrounded by smooth muscle, and lined with gastric epithelium. Endoscopic ultrasonography (EUS) is the most common method for diagnosis. Anechogenic lesions are monitored conservatively whereas hypoechogenic lesions may require endoscopic ultrasound with fine needle aspiration (EUS-FNA). Symptomatic duplication cysts tend to require surgical management. EUS-FNA has a higher infection rate; however, effectively rules out deceiving malignant lesions. There is controversy within the literature regarding whether to complete FNA to confirm duplication cyst. Our case series emphasizes taking risk-migrating steps to decrease infections and determine a diagnosis.
Case Description/Methods: An 89-year-old male was incidentally found to have a small paraesophageal nodule of approximately 3.4 cm on CT abdomen. After EUS-FNA, 5 mL of yellowish fluid was suctioned and analyzed by cytology. Cytology revealed benign squamous cells, macrophages, neutrophils, and amorphous material read into the diagnosis of esophageal duplication cyst.
A 75-year-old male presented with dysphagia. EGD revealed a 3.7 cm paraesophageal cyst. EUS-FNA confirmed EDC by aspirating 5mL; cytology was negative for malignancy and showed amorphous material.
Discussion: Mucin-filled cysts can appear hypoechoic rather than anechoic on EUS and CT values are within the range of soft tissue density. CT and MRI misdiagnose EDC as a solid lesion in about 70% of cases. CE-EUS could delineate malignant lesions and abscesses based on their vascular enhancement and rim enhancement. Duplication cysts have rim enhancement, whereas malignant lesions would grossly enhance. Avoiding aspiration would mitigate infection. Mediastinitis and abscess formation are major complications. Completing a repeat CE-EUS within 4-5 days with no change in echogenicity and size would decrease the suspicion of abscess development. Contrast-enhanced ultrasound in combination with endoscopic ultrasound (CE-EUS) can differentiate duplication cysts from a more ominous lesion by their vascular component without the need for biopsy. Monitoring changes in echogenicity and size of the EDC prior to symptoms would allow clinicians to start more aggressive treatment earlier.

Figure: Figure 1a and 1b: Case Report #1 EUS paraesophageal cyst found on EUS; Figure 2: Case Report #2 paraesophageal cyst found on EUS.
Disclosures:
Abu Fahad Abbasi indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Joshua Almaraj indicated no relevant financial relationships.
Filippa Trikantzopoulou indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Abu Fahad Abbasi, MD1, Fnu Vikash, MD2, Joshua Almaraj, MD3, Filippa Trikantzopoulou, MD4, Promila Banerjee, MD1. P3309 - Esophageal Duplication Cysts: Diagnostic Challenges and Risk-Mitigating Approaches, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
