Tuesday Poster Session
Category: Esophagus
P3316 - Unique Incidental Discovery of Burkitt’s Lymphoma in a Patient Presenting With Dysphagia
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PR
Pavithra Ramakrishnan, MS, MD
University of MInnesota
Minneapolis, MN
Presenting Author(s)
Pavithra Ramakrishnan, MS, MD1, Vijay S. Are, MD2, Cade Arries, MD2, Shahnaz Sultan, MD2
1University of MInnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN
Introduction: Gastrointestinal (GI) lymphomas comprise 1-4% of the malignant neoplasm in the GI tract of which < 1% are present in the esophagus. Having a robust differential for incidental subepithelial masses is critical before biopsy to plan for an adequate approach to sampling for subsequent diagnostics. Here we present a rare incidental discovery of Burkitt’s lymphoma (BL) while evaluating an immunocompetent patient with dysphagia.
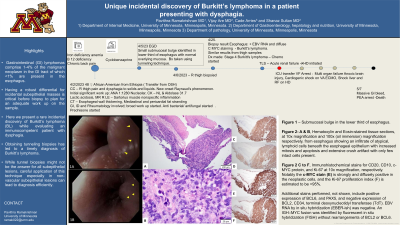
Case Description/Methods: A 48-year-old, previously healthy, woman originally from Ethiopia presented to the emergency department with 1-2 months of progressively worsening dysphagia and right leg swelling. Initial blood work was significant for lactic acidosis, elevated inflammatory markers and D dimer. Pertinent investigations computed tomography (CT) which demonstrated findings of esophagitis, gastritis, mediastinitis, proximal aortitis and myositis of thigh muscles. A broad autoimmune and infectious work up was obtained which include ANA 1:1280 with nucleolar pattern and elevated aldolase. Multisystem inflammatory or infectious process was considered as the primary differential. The patient was started empirically on broad spectrum antibiotics and 30 mg prednisone twice daily. She subsequently underwent an esophagogastroduodenoscopy which revealed a small submucosal bulge with overlying erythematous mucosa in the distal third of the esophagus. Biopsy samples targeting the subepithelial lesion were obtained using a tunneling technique (Figure 1). Distal esophagus biopsy samples showed > 95% Ki-67 proliferative index and strong diffuse cMyc staining suggestive of Burkitt’s lymphoma (Figure 2). The patient was ultimately diagnosed with Stage 4 Burkitt’s lymphoma. Serum EBV viral load was undetectable. Unfortunately, over the next 2 weeks, the patient developed tumor lysis syndrome, worsening kidney function and soon after initiation of chemotherapy, she suffered multiple complications which ultimately resulted in her passing away.
Discussion: Our case has several unique features, primarily being the first case of Burkitt’s lymphoma presenting as an esophageal subepithelial lesion. Obtaining tunneling biopsies led to a timely diagnosis of Burkitt’s lymphoma. While tunnel biopsies might not be the answer for all subepithelial lesions, careful application of this technique especially in non-vascular subepithelial lesions can lead to timely and efficient diagnosis.

Disclosures:
Pavithra Ramakrishnan, MS, MD1, Vijay S. Are, MD2, Cade Arries, MD2, Shahnaz Sultan, MD2. P3316 - Unique Incidental Discovery of Burkitt’s Lymphoma in a Patient Presenting With Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of MInnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN
Introduction: Gastrointestinal (GI) lymphomas comprise 1-4% of the malignant neoplasm in the GI tract of which < 1% are present in the esophagus. Having a robust differential for incidental subepithelial masses is critical before biopsy to plan for an adequate approach to sampling for subsequent diagnostics. Here we present a rare incidental discovery of Burkitt’s lymphoma (BL) while evaluating an immunocompetent patient with dysphagia.
Case Description/Methods: A 48-year-old, previously healthy, woman originally from Ethiopia presented to the emergency department with 1-2 months of progressively worsening dysphagia and right leg swelling. Initial blood work was significant for lactic acidosis, elevated inflammatory markers and D dimer. Pertinent investigations computed tomography (CT) which demonstrated findings of esophagitis, gastritis, mediastinitis, proximal aortitis and myositis of thigh muscles. A broad autoimmune and infectious work up was obtained which include ANA 1:1280 with nucleolar pattern and elevated aldolase. Multisystem inflammatory or infectious process was considered as the primary differential. The patient was started empirically on broad spectrum antibiotics and 30 mg prednisone twice daily. She subsequently underwent an esophagogastroduodenoscopy which revealed a small submucosal bulge with overlying erythematous mucosa in the distal third of the esophagus. Biopsy samples targeting the subepithelial lesion were obtained using a tunneling technique (Figure 1). Distal esophagus biopsy samples showed > 95% Ki-67 proliferative index and strong diffuse cMyc staining suggestive of Burkitt’s lymphoma (Figure 2). The patient was ultimately diagnosed with Stage 4 Burkitt’s lymphoma. Serum EBV viral load was undetectable. Unfortunately, over the next 2 weeks, the patient developed tumor lysis syndrome, worsening kidney function and soon after initiation of chemotherapy, she suffered multiple complications which ultimately resulted in her passing away.
Discussion: Our case has several unique features, primarily being the first case of Burkitt’s lymphoma presenting as an esophageal subepithelial lesion. Obtaining tunneling biopsies led to a timely diagnosis of Burkitt’s lymphoma. While tunnel biopsies might not be the answer for all subepithelial lesions, careful application of this technique especially in non-vascular subepithelial lesions can lead to timely and efficient diagnosis.

Figure: Figure 1A&B – Submucosal bulge in the lower third of esophagus. Figure 2 - A &; B, Hematoxylin and Eosin-stained tissue sections, at 10x magnification and 100x (oil immersion) magnification respectively, from esophagus showing an infiltrate of atypical,lymphoid cells beneath the esophageal epithelium with increased mitosis and apoptosis and extensive crush artifact with only few intact cells present. C to F, Immunohistochemical stains for CD20, CD10, c-MYC protein, and Ki-67 at 10x magnification, respectively. Notably the c-MYC stain (E) is strongly and diffusely positive in the neoplastic cells, and the Ki-67 proliferation index (F) is estimated to be 95%. Additional stains performed, not shown, include positive expression of BCL6, and PAX5, and negative expression of BCL2, CD34, terminal deoxynucleotidyl transferase (TdT). EBV RNA by in situ hybridization (EBER-ish) was negative. An IGH::MYC fusion was identified by fluorescent in situ hybridization (FISH) without rearrangements of BCL2 or BCL6.
Disclosures:
Pavithra Ramakrishnan indicated no relevant financial relationships.
Vijay Are indicated no relevant financial relationships.
Cade Arries indicated no relevant financial relationships.
Shahnaz Sultan indicated no relevant financial relationships.
Pavithra Ramakrishnan, MS, MD1, Vijay S. Are, MD2, Cade Arries, MD2, Shahnaz Sultan, MD2. P3316 - Unique Incidental Discovery of Burkitt’s Lymphoma in a Patient Presenting With Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
