Tuesday Poster Session
Category: Esophagus
P3320 - Management of Acute Esophageal Necrosis With Perforation Using Esophageal Stents to Prevent Resection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- JK
Judah Kupferman, MD
Icahn School of Medicine at Mount Sinai, NYC Health + Hospitals/Elmhurst
Queens, NY
Presenting Author(s)
Judah Kupferman, MD1, Sindhura Kolli, MD2, Krishna Gurram, MD1
1Icahn School of Medicine at Mount Sinai, NYC Health + Hospitals/Elmhurst, Queens, NY; 2Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: While surgery has long been the default answer to esophageal perforations, the emergence of self-expanding metallic stents (SEMS) are competing as a viable alternative to an esophagectomy. Our atypical case of acute esophageal necrosis with a perforation was remedied by esophageal stents preserving quality of life.
Case Description/Methods: A 52 year old African male with alcohol use disorder and erosive esophagitis presented with five days of emesis. He was tachycardic to 125 bpm, and his physical exam was otherwise unremarkable. Abnormal labs included an elevated lactate of 2.0 mmol/L and WBC of 14,000/mcL. An abdominal computed tomography (CT) scan revealed a necrotic stomach wall and a perforation in the lower esophagus.
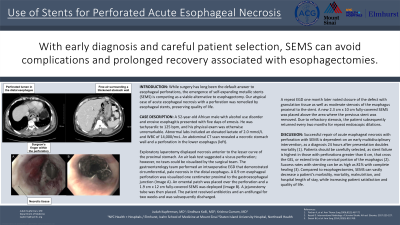
Exploratory laparotomy displayed necrosis anterior to the lesser curve of the proximal stomach. An air leak test suggested viscus perforation; however, no tears could be visualized by the surgical team. Gastroenterology performed an intraoperative esophagogastroduodenoscopy (EGD) which noted circumferential, pale necrosis in the distal esophagus. A 0.9 centimeter (cm) esophageal perforation was visualized 1 cm proximal to the gastroesophageal junction (GEJ) (Image A). An omental patch was placed over the perforation and a 1.9 cm x 12 cm fully-covered SEMS was deployed (Image B). A jejunostomy tube was then placed. The patient received antibiotics and an antifungal for two weeks and was subsequently discharged.
A repeat EGD one month later noted closure of the defect by granulation tissue as well as moderate stenosis of the esophagus proximal to the stent. A new 2.3 cm x 10 cm fully-covered SEMS was placed above the area where the previous stent was removed. Due to refractory stenosis, the patient subsequently returned every two months for repeat endoscopic dilations.
Discussion: Successful repair of acute esophageal necrosis with esophageal perforation with SEMS is dependent on an early multidisciplinary intervention, as a diagnosis 24 hours after presentation doubles mortality. Patients should be carefully selected, as stent failure is highest in those with perforations greater than 6 cm, that cross the GEJ, or extend into the cervical portion of the esophagus. Compared to esophagectomy, SEMS can vastly decrease the morbidity, mortality, malnutrition, hospital length of stay, while increasing patient satisfaction and quality of life.

Disclosures:
Judah Kupferman, MD1, Sindhura Kolli, MD2, Krishna Gurram, MD1. P3320 - Management of Acute Esophageal Necrosis With Perforation Using Esophageal Stents to Prevent Resection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, NYC Health + Hospitals/Elmhurst, Queens, NY; 2Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: While surgery has long been the default answer to esophageal perforations, the emergence of self-expanding metallic stents (SEMS) are competing as a viable alternative to an esophagectomy. Our atypical case of acute esophageal necrosis with a perforation was remedied by esophageal stents preserving quality of life.
Case Description/Methods: A 52 year old African male with alcohol use disorder and erosive esophagitis presented with five days of emesis. He was tachycardic to 125 bpm, and his physical exam was otherwise unremarkable. Abnormal labs included an elevated lactate of 2.0 mmol/L and WBC of 14,000/mcL. An abdominal computed tomography (CT) scan revealed a necrotic stomach wall and a perforation in the lower esophagus.
Exploratory laparotomy displayed necrosis anterior to the lesser curve of the proximal stomach. An air leak test suggested viscus perforation; however, no tears could be visualized by the surgical team. Gastroenterology performed an intraoperative esophagogastroduodenoscopy (EGD) which noted circumferential, pale necrosis in the distal esophagus. A 0.9 centimeter (cm) esophageal perforation was visualized 1 cm proximal to the gastroesophageal junction (GEJ) (Image A). An omental patch was placed over the perforation and a 1.9 cm x 12 cm fully-covered SEMS was deployed (Image B). A jejunostomy tube was then placed. The patient received antibiotics and an antifungal for two weeks and was subsequently discharged.
A repeat EGD one month later noted closure of the defect by granulation tissue as well as moderate stenosis of the esophagus proximal to the stent. A new 2.3 cm x 10 cm fully-covered SEMS was placed above the area where the previous stent was removed. Due to refractory stenosis, the patient subsequently returned every two months for repeat endoscopic dilations.
Discussion: Successful repair of acute esophageal necrosis with esophageal perforation with SEMS is dependent on an early multidisciplinary intervention, as a diagnosis 24 hours after presentation doubles mortality. Patients should be carefully selected, as stent failure is highest in those with perforations greater than 6 cm, that cross the GEJ, or extend into the cervical portion of the esophagus. Compared to esophagectomy, SEMS can vastly decrease the morbidity, mortality, malnutrition, hospital length of stay, while increasing patient satisfaction and quality of life.

Figure: Endoscopic images of the distal esophagus with white necrotic tissue. On the left (A), the surgeon’s gloved finger can be seen penetrating through the perforated lumen. On the right (B), a fully-covered stent has been placed following omental patching.
Disclosures:
Judah Kupferman indicated no relevant financial relationships.
Sindhura Kolli indicated no relevant financial relationships.
Krishna Gurram indicated no relevant financial relationships.
Judah Kupferman, MD1, Sindhura Kolli, MD2, Krishna Gurram, MD1. P3320 - Management of Acute Esophageal Necrosis With Perforation Using Esophageal Stents to Prevent Resection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

