Tuesday Poster Session
Category: Esophagus
P3347 - Esophageal Perforation in Hypermobile Ehlers Danlos Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- ES
Elisha Shah, DO
Baystate Medical Center
Springfield, MA
Presenting Author(s)
Elisha Shah, DO1, Sherin Samuel, DO2, Yesenia Greeff, MD2
1Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School-Baystate, Springfield, MA
Introduction: Ehlers-Danlos Syndrome (EDS) is an inherited connective tissue disorder resulting from defects in synthesis of collagen. Well known clinical manifestations include those affecting the skin, joints, and blood vessels. Gastrointestinal (GI) symptoms typically seen in EDS patients include abdominal pain, nausea, and heartburn. Rarely, perforation of GI organs occurs in the vascular subtype of EDS in either the colon or small intestine. We present a rare case of esophageal perforation in a young female with hypermobile EDS.
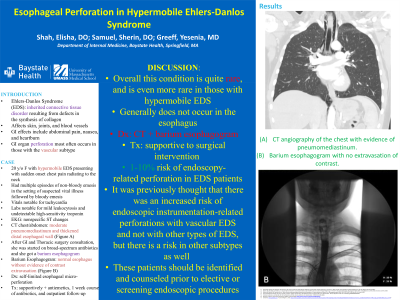
Case Description/Methods: A 20-year-old female with medical history of hypermobile EDS presented to the hospital with sudden onset chest pain radiating to her neck. She had multiple episodes of non-bloody emesis in the prior 24 hours, with known sick contacts, and had been unable to tolerate oral intake for the past day. She was tachycardic. Electrocardiogram showed non-specific ST changes, with no baseline for comparison. Labs showed mild leukocytosis and undetectable high-sensitivity troponin, without any electrolyte abnormalities. Physical examination was unremarkable. Chest radiograph was unremarkable. Computed tomography (CT) of chest and abdomen was negative for aortic aneurysm or dissection, but revealed moderate pneumomediastinum and thickened distal esophageal wall. Gastroenterology and Thoracic Surgery were consulted and recommended broad-spectrum antibiotics and a barium esophagogram. The study revealed a normal esophagus without evidence of contrast extravasation. Given the patient’s findings on imaging and improvement in symptoms, self-limited esophageal micro-perforation was suspected. Inpatient endoscopic evaluation was deferred. The patient was managed supportively, and was able to tolerate advancement of diet. She was discharged with antiemetics, one-week course of antibiotics, and outpatient follow-up.
Discussion: GI perforation is a rare and dangerous manifestation of EDS and presents even more infrequently in the esophagus and in the hypermobile subtype of EDS. A study of safety outcomes revealed 1-10% risk of endoscopy-related perforation in the EDS population. Noninvasive testing such as CT and barium esophagogram can provide diagnostic confirmation. Treatment can range from supportive management to surgical intervention. Clinicians should be aware that GI perforations in EDS can occur in any GI organ and in non-vascular subtypes, as delays in diagnosis can lead to adverse outcomes.
Disclosures:
Elisha Shah, DO1, Sherin Samuel, DO2, Yesenia Greeff, MD2. P3347 - Esophageal Perforation in Hypermobile Ehlers Danlos Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School-Baystate, Springfield, MA
Introduction: Ehlers-Danlos Syndrome (EDS) is an inherited connective tissue disorder resulting from defects in synthesis of collagen. Well known clinical manifestations include those affecting the skin, joints, and blood vessels. Gastrointestinal (GI) symptoms typically seen in EDS patients include abdominal pain, nausea, and heartburn. Rarely, perforation of GI organs occurs in the vascular subtype of EDS in either the colon or small intestine. We present a rare case of esophageal perforation in a young female with hypermobile EDS.
Case Description/Methods: A 20-year-old female with medical history of hypermobile EDS presented to the hospital with sudden onset chest pain radiating to her neck. She had multiple episodes of non-bloody emesis in the prior 24 hours, with known sick contacts, and had been unable to tolerate oral intake for the past day. She was tachycardic. Electrocardiogram showed non-specific ST changes, with no baseline for comparison. Labs showed mild leukocytosis and undetectable high-sensitivity troponin, without any electrolyte abnormalities. Physical examination was unremarkable. Chest radiograph was unremarkable. Computed tomography (CT) of chest and abdomen was negative for aortic aneurysm or dissection, but revealed moderate pneumomediastinum and thickened distal esophageal wall. Gastroenterology and Thoracic Surgery were consulted and recommended broad-spectrum antibiotics and a barium esophagogram. The study revealed a normal esophagus without evidence of contrast extravasation. Given the patient’s findings on imaging and improvement in symptoms, self-limited esophageal micro-perforation was suspected. Inpatient endoscopic evaluation was deferred. The patient was managed supportively, and was able to tolerate advancement of diet. She was discharged with antiemetics, one-week course of antibiotics, and outpatient follow-up.
Discussion: GI perforation is a rare and dangerous manifestation of EDS and presents even more infrequently in the esophagus and in the hypermobile subtype of EDS. A study of safety outcomes revealed 1-10% risk of endoscopy-related perforation in the EDS population. Noninvasive testing such as CT and barium esophagogram can provide diagnostic confirmation. Treatment can range from supportive management to surgical intervention. Clinicians should be aware that GI perforations in EDS can occur in any GI organ and in non-vascular subtypes, as delays in diagnosis can lead to adverse outcomes.
Disclosures:
Elisha Shah indicated no relevant financial relationships.
Sherin Samuel indicated no relevant financial relationships.
Yesenia Greeff indicated no relevant financial relationships.
Elisha Shah, DO1, Sherin Samuel, DO2, Yesenia Greeff, MD2. P3347 - Esophageal Perforation in Hypermobile Ehlers Danlos Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
