Tuesday Poster Session
Category: Esophagus
P3354 - An Unsuspecting Case of Dysphagia: Chagas Esophageal Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Benjamin Chipkin, MD, MS
Yale University School of Medicine
New Haven, CT
Presenting Author(s)
Benjamin Chipkin, MD, MS1, Badr Al-Bawardy, MD2
1Yale University School of Medicine, New Haven, CT; 2King Faisal Specialist Hospital and Research Center, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Chagas disease (CD) is most common in Central and South America, or in people with travel to endemic regions. In chronic CD, cardiac and gastrointestinal (GI) involvement occurs in 30% and 10-21% of cases, respectively. Esophageal disease mimics idiopathic achalasia, and colonic disease results in progressive dilation. We present a case of a woman in the Northeastern United States (US) with cardiac and GI manifestations of CD.
Case Description/Methods: We cared for a 70-year-old woman who immigrated to the US from Honduras with history of nonischemic cardiomyopathy (NICM) with reduced ejection fraction (11%) and gastrointestinal reflux disease who presented with acute decompensated heart failure. She was treated successfully with diuretics. After stabilization, she noted difficulty swallowing with sensation of food stuck in her chest a few seconds after ingestion, which started with solid foods eight years earlier and progressed to liquids over the past year. It was associated with weight loss and reflux, for which she used a daily proton pump inhibitor. She denied coughing with eating, nausea, and vomiting. CT of chest and abdomen showed cardiomegaly with possible esophageal compression. Esophagram showed abnormal esophageal motility with markedly delayed emptying through lower esophageal sphincter, suggesting an achalasia-like process, rather than extrinsic compression.
She wished to transition to palliative care considering her end-stage heart failure diagnosis; however, she was open to minimally invasive procedures for palliation of dysphagia symptoms given her desire to enjoy “homestyle Honduran food.” Esophagogastroduodenoscopy (EGD) showed normal esophageal appearance with no resistance traversing the gastroesophageal junction (GEJ). Empiric botulinum toxin injections were given at the GEJ for suspected dysmotility. Subsequently, Trypanosoma cruzi antibody was positive. Her NICM and dysphagia were suspected to be manifestations of CD. Unfortunately, she died of decompensated heart failure before her dysphagia could be adequately followed up outpatient.
Discussion: Chagas GI disease can have considerable impact on quality of life, and given the lack of efficacy for antitrypanosomals, symptomatic management is the mainstay. We should consider CD in adults with esophageal dysphagia and concomitant NICM. Although CD predominates in Central and South America, climate change may drive endemic areas further north, where clinical suspicion remains low.

Disclosures:
Benjamin Chipkin, MD, MS1, Badr Al-Bawardy, MD2. P3354 - An Unsuspecting Case of Dysphagia: Chagas Esophageal Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale University School of Medicine, New Haven, CT; 2King Faisal Specialist Hospital and Research Center, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Chagas disease (CD) is most common in Central and South America, or in people with travel to endemic regions. In chronic CD, cardiac and gastrointestinal (GI) involvement occurs in 30% and 10-21% of cases, respectively. Esophageal disease mimics idiopathic achalasia, and colonic disease results in progressive dilation. We present a case of a woman in the Northeastern United States (US) with cardiac and GI manifestations of CD.
Case Description/Methods: We cared for a 70-year-old woman who immigrated to the US from Honduras with history of nonischemic cardiomyopathy (NICM) with reduced ejection fraction (11%) and gastrointestinal reflux disease who presented with acute decompensated heart failure. She was treated successfully with diuretics. After stabilization, she noted difficulty swallowing with sensation of food stuck in her chest a few seconds after ingestion, which started with solid foods eight years earlier and progressed to liquids over the past year. It was associated with weight loss and reflux, for which she used a daily proton pump inhibitor. She denied coughing with eating, nausea, and vomiting. CT of chest and abdomen showed cardiomegaly with possible esophageal compression. Esophagram showed abnormal esophageal motility with markedly delayed emptying through lower esophageal sphincter, suggesting an achalasia-like process, rather than extrinsic compression.
She wished to transition to palliative care considering her end-stage heart failure diagnosis; however, she was open to minimally invasive procedures for palliation of dysphagia symptoms given her desire to enjoy “homestyle Honduran food.” Esophagogastroduodenoscopy (EGD) showed normal esophageal appearance with no resistance traversing the gastroesophageal junction (GEJ). Empiric botulinum toxin injections were given at the GEJ for suspected dysmotility. Subsequently, Trypanosoma cruzi antibody was positive. Her NICM and dysphagia were suspected to be manifestations of CD. Unfortunately, she died of decompensated heart failure before her dysphagia could be adequately followed up outpatient.
Discussion: Chagas GI disease can have considerable impact on quality of life, and given the lack of efficacy for antitrypanosomals, symptomatic management is the mainstay. We should consider CD in adults with esophageal dysphagia and concomitant NICM. Although CD predominates in Central and South America, climate change may drive endemic areas further north, where clinical suspicion remains low.

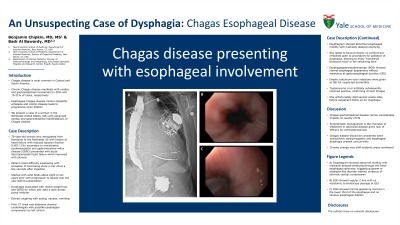
Figure: (A) Esophagram showing abnormal motility with markedly delayed emptying through the lower esophageal sphincter, suggesting underlying spasm or achalasia-like equivalent. No evidence of extrinsic cardiac compression from left atrium. (B) EGD showing regular Z-line with no resistance to endoscope passage through the GEJ. (C) EGD showing normal-appearing mucosa in the lower third of the esophagus and no obvious esophageal dilation.
Disclosures:
Benjamin Chipkin indicated no relevant financial relationships.
Badr Al-Bawardy: AbbVie – Speakers Bureau. Bristol Myers Squibb – Advisor or Review Panel Member, Speakers Bureau. Pfizer – Advisor or Review Panel Member. Takeda – Speakers Bureau.
Benjamin Chipkin, MD, MS1, Badr Al-Bawardy, MD2. P3354 - An Unsuspecting Case of Dysphagia: Chagas Esophageal Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
