Tuesday Poster Session
Category: General Endoscopy
P3414 - Unmasking Ampullary High-Grade Dysplasia in Li-Fraumeni Syndrome: A Call for Vigilant Surveillance
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MK
Michelle H. Kwon, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Michelle H. Kwon, MD1, Kaavya Mandi, MD1, Kanhai Farrakhan, MD1, Harlan Rich, MD2
1Warren Alpert Medical School of Brown University, Providence, RI; 2Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Li-Fraumeni syndrome is an autosomal dominant condition caused by a germline mutation in the TP53 gene, resulting in an increased susceptibility to various early-onset primary cancers. Due to significantly elevated cancer risk in these patients compared to the general population, routine surveillance for gastrointestinal (GI) cancer requires heightened vigilance. While the guidelines issued by the National Comprehensive Cancer Network recommend colonoscopy in patients with Li-Fraumeni syndrome, there is no explicit mention of the use of upper endoscopy (EGD). To highlight the potential significance of incorporating EGD into surveillance protocols for these individuals, we present a case of a 47-year-old male with a history of Li-Fraumeni syndrome who was found to have an ampullary adenoma with high-grade dysplasia detected during EGD.
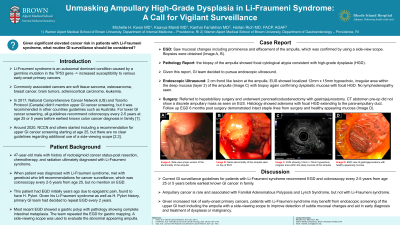
Case Description/Methods: A 47-year-old male with past medical history of rectal cancer status-post resection, chemotherapy, and radiation ultimately diagnosed with Li-Fraumeni syndrome through genetic testing presented for a surveillance EGD. He had prior undergone an EGD for epigastric pain which demonstrated a gastric polyp and gastric biopsies revealing complete intestinal metaplasia, prompting the primary GI team to pursue gastric mapping. The surveillance EGD revealed mucosal changes and prominent effacement of ampulla (Image 1). This was confirmed using side-view scope and biopsies that were obtained revealed focal primarily cytological atypia consistent with high-grade dysplasia. Subsequent endoscopic ultrasound showed a localized 12mm x 15mm hypoechoic, irregular area within the deep mucosa (layer 2) of the ampulla (Image 2), with biopsy confirming dysplastic mucosa with focal high-grade dysplasia. The patient was referred to hepatobiliary surgery for resection of the ampullary mass and underwent pancreaticoduodenectomy. Six months post-surgery a follow-up EGD demonstrated intact staple lines from the surgery and healthy appearing mucosa.
Discussion: While primary ampullary malignancies are rare, this case highlights the importance of vigilant surveillance in patients with Li-Fraumeni syndrome. Due to their predisposition to multiple primary malignancies these patients likely would benefit from upper GI screening in addition to colonoscopies. Endoscopic screening of the upper GI tract, including the ampulla with side-view scope, could improve detection of subtle mucosal changes and aid in early diagnosis and treatment of dysplasia or malignancy.

Disclosures:
Michelle H. Kwon, MD1, Kaavya Mandi, MD1, Kanhai Farrakhan, MD1, Harlan Rich, MD2. P3414 - Unmasking Ampullary High-Grade Dysplasia in Li-Fraumeni Syndrome: A Call for Vigilant Surveillance, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University, Providence, RI; 2Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Li-Fraumeni syndrome is an autosomal dominant condition caused by a germline mutation in the TP53 gene, resulting in an increased susceptibility to various early-onset primary cancers. Due to significantly elevated cancer risk in these patients compared to the general population, routine surveillance for gastrointestinal (GI) cancer requires heightened vigilance. While the guidelines issued by the National Comprehensive Cancer Network recommend colonoscopy in patients with Li-Fraumeni syndrome, there is no explicit mention of the use of upper endoscopy (EGD). To highlight the potential significance of incorporating EGD into surveillance protocols for these individuals, we present a case of a 47-year-old male with a history of Li-Fraumeni syndrome who was found to have an ampullary adenoma with high-grade dysplasia detected during EGD.
Case Description/Methods: A 47-year-old male with past medical history of rectal cancer status-post resection, chemotherapy, and radiation ultimately diagnosed with Li-Fraumeni syndrome through genetic testing presented for a surveillance EGD. He had prior undergone an EGD for epigastric pain which demonstrated a gastric polyp and gastric biopsies revealing complete intestinal metaplasia, prompting the primary GI team to pursue gastric mapping. The surveillance EGD revealed mucosal changes and prominent effacement of ampulla (Image 1). This was confirmed using side-view scope and biopsies that were obtained revealed focal primarily cytological atypia consistent with high-grade dysplasia. Subsequent endoscopic ultrasound showed a localized 12mm x 15mm hypoechoic, irregular area within the deep mucosa (layer 2) of the ampulla (Image 2), with biopsy confirming dysplastic mucosa with focal high-grade dysplasia. The patient was referred to hepatobiliary surgery for resection of the ampullary mass and underwent pancreaticoduodenectomy. Six months post-surgery a follow-up EGD demonstrated intact staple lines from the surgery and healthy appearing mucosa.
Discussion: While primary ampullary malignancies are rare, this case highlights the importance of vigilant surveillance in patients with Li-Fraumeni syndrome. Due to their predisposition to multiple primary malignancies these patients likely would benefit from upper GI screening in addition to colonoscopies. Endoscopic screening of the upper GI tract, including the ampulla with side-view scope, could improve detection of subtle mucosal changes and aid in early diagnosis and treatment of dysplasia or malignancy.

Figure: Image 1: EGD view of abnormal mucosa at the ampulla
Image 2: 12mm x 15mm ampulla mass on endoscopic ultrasound
Image 2: 12mm x 15mm ampulla mass on endoscopic ultrasound
Disclosures:
Michelle Kwon indicated no relevant financial relationships.
Kaavya Mandi indicated no relevant financial relationships.
Kanhai Farrakhan indicated no relevant financial relationships.
Harlan Rich indicated no relevant financial relationships.
Michelle H. Kwon, MD1, Kaavya Mandi, MD1, Kanhai Farrakhan, MD1, Harlan Rich, MD2. P3414 - Unmasking Ampullary High-Grade Dysplasia in Li-Fraumeni Syndrome: A Call for Vigilant Surveillance, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
