Tuesday Poster Session
Category: GI Bleeding
P3461 - Comparative Analysis of Concurrent Clostridium difficile Infection on Hospitalization Outcomes in Variceal vs Non-Variceal Upper Gastrointestinal Bleeding: National Inpatient Sample Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Harshavardhan Sanekommu, MD
Hackensack Meridian Jersey Shore University Medical Center
Neptune, NJ
Presenting Author(s)
Harshavardhan Sanekommu, MD1, Sobaan Taj, MD1, Jayasree Ravilla, MD2, Aidan Farrell, BS3, Rida Mah Noor, BS4, Muhammad Umair Akmal, BS5, Reza Akhtar, MD3, Mohammad Hossain, MD3, Arif Asif, MD, MBA, MAS3
1Hackensack Meridian Jersey Shore University Medical Center, Neptune, NJ; 2Monmouth Medical Center/RWJBH, Long Branch, NJ; 3Hackensack Meridian Jersey Shore University Medical Center, Neptune Township, NJ; 4International University of Kyrgyzstan, International School of Medicine, Bishkek, Bishkek, Kyrgyzstan; 5Kazakh National Medical University, Almaty, Almaty, Kazakhstan
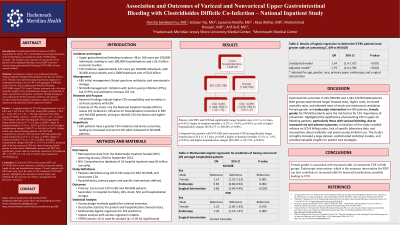
Introduction: Clostridium difficile infections (CDI) significantly affect hospitalizations, leading to considerable mortality and morbidity. However, the impact of CDI on non-variceal bleeding remains unexplored as most research focuses on variceal bleeding. This study aims to compare the outcomes of CDI in variceal and non-variceal bleeding cases and investigate if variceal bleeding patients have a higher likelihood of developing CDI.
Methods: Retrospective analysis was performed using National Inpatient Sample (NIS) from years 2010 to September 2015. Patients were identified using the primary diagnosis of esophageal variceal bleeding and aggregate of different sources of non-variceal bleeding using ICD-9 codes. Primary outcomes were, all-cause mortality, length of stay, hospitalization charges, development of shock, and need for mechanical ventilation. Statistical analysis was conducted by STATA statistical software and analyses included multivariate logistic regression, negative binomial regression and generalized linear regression models.
Results: A weighted number of 225,708 hospitalizations were for variceal bleeding and 1,342,724 for non-variceal bleeding. Among variceal bleeding patients, 1.64% (n = 3,696, 95% CI: 1.52 - 1.76) had concurrent CDI, while among non-variceal bleeding patients, 1.07% (n = 14,390, 95% CI: 1.03 - 1.12) had CDI. Patients with variceal bleeding and CDI had significantly longer hospital stays (14.7 vs. 6.2 days, p< 0.001), higher in-hospital mortality (15.2% vs. 10.0%, p< 0.001), increased rates of shock (24.6% vs. 13.1%, p< 0.001) and mechanical ventilation (32.7% vs. 17.3%, p< 0.001), as well as higher hospitalization charges ($168,275 vs. $68,446, p< 0.001). Similar trends were observed among patients with non-variceal bleeding. Comparatively, patients with concurrent CDI had significantly longer hospital stays (10.6 vs. 4.3 days, p< 0.001), higher in-hospital mortality (5.5% vs. 1.9%, p< 0.001), increased rates of shock (13.1% vs. 5.0%, p< 0.001) and mechanical ventilation (12.0% vs. 3.3%, p< 0.001), as well as higher hospitalization charges ($92,480 vs. $37,553, p< 0.001). When compared with non-variceal bleeding patients, patients with variceal bleeding patients had significantly greater odds of contracting concurrent C. difficile infection (adjusted OR: 1.79; 95% CI: 1.60-1.98, p< 0.001).
Discussion: Concurrent CDI for both variceal and non-variceal bleeding groups leads to worser outcomes. Esophageal variceal group has greater odds of developing CDI.
Disclosures:
Harshavardhan Sanekommu, MD1, Sobaan Taj, MD1, Jayasree Ravilla, MD2, Aidan Farrell, BS3, Rida Mah Noor, BS4, Muhammad Umair Akmal, BS5, Reza Akhtar, MD3, Mohammad Hossain, MD3, Arif Asif, MD, MBA, MAS3. P3461 - Comparative Analysis of Concurrent Clostridium difficile Infection on Hospitalization Outcomes in Variceal vs Non-Variceal Upper Gastrointestinal Bleeding: National Inpatient Sample Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Hackensack Meridian Jersey Shore University Medical Center, Neptune, NJ; 2Monmouth Medical Center/RWJBH, Long Branch, NJ; 3Hackensack Meridian Jersey Shore University Medical Center, Neptune Township, NJ; 4International University of Kyrgyzstan, International School of Medicine, Bishkek, Bishkek, Kyrgyzstan; 5Kazakh National Medical University, Almaty, Almaty, Kazakhstan
Introduction: Clostridium difficile infections (CDI) significantly affect hospitalizations, leading to considerable mortality and morbidity. However, the impact of CDI on non-variceal bleeding remains unexplored as most research focuses on variceal bleeding. This study aims to compare the outcomes of CDI in variceal and non-variceal bleeding cases and investigate if variceal bleeding patients have a higher likelihood of developing CDI.
Methods: Retrospective analysis was performed using National Inpatient Sample (NIS) from years 2010 to September 2015. Patients were identified using the primary diagnosis of esophageal variceal bleeding and aggregate of different sources of non-variceal bleeding using ICD-9 codes. Primary outcomes were, all-cause mortality, length of stay, hospitalization charges, development of shock, and need for mechanical ventilation. Statistical analysis was conducted by STATA statistical software and analyses included multivariate logistic regression, negative binomial regression and generalized linear regression models.
Results: A weighted number of 225,708 hospitalizations were for variceal bleeding and 1,342,724 for non-variceal bleeding. Among variceal bleeding patients, 1.64% (n = 3,696, 95% CI: 1.52 - 1.76) had concurrent CDI, while among non-variceal bleeding patients, 1.07% (n = 14,390, 95% CI: 1.03 - 1.12) had CDI. Patients with variceal bleeding and CDI had significantly longer hospital stays (14.7 vs. 6.2 days, p< 0.001), higher in-hospital mortality (15.2% vs. 10.0%, p< 0.001), increased rates of shock (24.6% vs. 13.1%, p< 0.001) and mechanical ventilation (32.7% vs. 17.3%, p< 0.001), as well as higher hospitalization charges ($168,275 vs. $68,446, p< 0.001). Similar trends were observed among patients with non-variceal bleeding. Comparatively, patients with concurrent CDI had significantly longer hospital stays (10.6 vs. 4.3 days, p< 0.001), higher in-hospital mortality (5.5% vs. 1.9%, p< 0.001), increased rates of shock (13.1% vs. 5.0%, p< 0.001) and mechanical ventilation (12.0% vs. 3.3%, p< 0.001), as well as higher hospitalization charges ($92,480 vs. $37,553, p< 0.001). When compared with non-variceal bleeding patients, patients with variceal bleeding patients had significantly greater odds of contracting concurrent C. difficile infection (adjusted OR: 1.79; 95% CI: 1.60-1.98, p< 0.001).
Discussion: Concurrent CDI for both variceal and non-variceal bleeding groups leads to worser outcomes. Esophageal variceal group has greater odds of developing CDI.
Disclosures:
Harshavardhan Sanekommu indicated no relevant financial relationships.
Sobaan Taj indicated no relevant financial relationships.
Jayasree Ravilla indicated no relevant financial relationships.
Aidan Farrell indicated no relevant financial relationships.
Rida Mah Noor indicated no relevant financial relationships.
Muhammad Umair Akmal indicated no relevant financial relationships.
Reza Akhtar indicated no relevant financial relationships.
Mohammad Hossain indicated no relevant financial relationships.
Arif Asif indicated no relevant financial relationships.
Harshavardhan Sanekommu, MD1, Sobaan Taj, MD1, Jayasree Ravilla, MD2, Aidan Farrell, BS3, Rida Mah Noor, BS4, Muhammad Umair Akmal, BS5, Reza Akhtar, MD3, Mohammad Hossain, MD3, Arif Asif, MD, MBA, MAS3. P3461 - Comparative Analysis of Concurrent Clostridium difficile Infection on Hospitalization Outcomes in Variceal vs Non-Variceal Upper Gastrointestinal Bleeding: National Inpatient Sample Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
