Tuesday Poster Session
Category: GI Bleeding
P3463 - Acute GI Bleed Following CABG With Atrial Fibrillation on Antiplatelet and Anticoagulant
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- WR
Winnie Roy, MD, MPH
West Virginia University Camden Clark Medical Center
Parkersburg, West Virginia
Presenting Author(s)
Winnie Roy, MD, MPH, Umer Rizwan, MD, Mohamed Barakat, MD
West Virginia University Camden Clark Medical Center, Parkersburg, WV
Introduction: The risk of gastrointestinal bleeding (GIB) while on dual antiplatelets (AP) in patients after coronary artery bypass surgery (CABG) and post operative atrial fibrillation (PAOF) requiring oral anticoagulants (OC) is well known. The objective of this study is to determine the truth of this effect with anticoagulants across multiple health care organizations, and to see the need to do treatment interventions in these patient populations.
Methods: The data used for this study was collected from the TriNetX Network, which provided access to electronic medical records. We compared the data available in patients with CABG or POAF using AP and OC versus patients using AP only. The incidence of GIB in both these group were sought out. The number of these patients with GIB requiring transfusions, esophagogastroduodenoscopy (EGD) or interventional radiology embolization (IRE) were determined. The Odds ratio (OR) and Relative Risk (RR) in these groups with 95% Confidence Interval (CI) were calculated using statistical software. This was also examined for a p-value of < 0.05 significance.
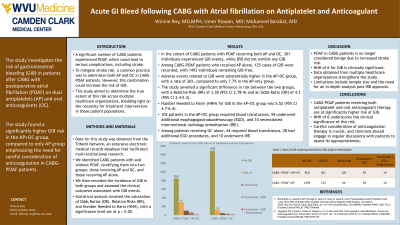
Results: In CABG with POAF using AP and OC there was 301 with GIB events and 850 without any GIB. CABG with POAF using OC only 125 had GIB events while 1493 did not have any GIB events. Adverse events noted in the AP+ OC group was 26%, vs 7.7% patients in the AP group. The RR between the groups were 3.38 95% CI (2.78-4) with p-value < 0.0001. OR between the groups was 4.2; 95% CI (3.4-5.3). Number needed to harm (NNH) or cause GIB was 6; 95% CI (4.7- 6.4).
In the group with AP and OC 102 patients got blood transfusions, 59 received additional EGD and 10 required IRE eventually. The group with OC use, 44 patients got blood transfusions, 28 got EGD additionally and 10 required IRE eventually.
Discussion: The incidence of GIB as expected is more with AP and OC together in patients with CABG and POAF. NNH of 6 is high causing a GIB. Strengths of this study is that the data was obtained from multiple healthcare organizations. Limitations of this study is that an in-depth analysis of patient data and chronologic events was beyond the scope of this study. Detailed review after IRB approval is pending.
A need to stop, adjust or reconsider anticoagulation in patients with CABG and POAF is an important clinical decision that needs to be constantly addressed on subsequent visits between the clinician and the patient.

Disclosures:
Winnie Roy, MD, MPH, Umer Rizwan, MD, Mohamed Barakat, MD. P3463 - Acute GI Bleed Following CABG With Atrial Fibrillation on Antiplatelet and Anticoagulant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
West Virginia University Camden Clark Medical Center, Parkersburg, WV
Introduction: The risk of gastrointestinal bleeding (GIB) while on dual antiplatelets (AP) in patients after coronary artery bypass surgery (CABG) and post operative atrial fibrillation (PAOF) requiring oral anticoagulants (OC) is well known. The objective of this study is to determine the truth of this effect with anticoagulants across multiple health care organizations, and to see the need to do treatment interventions in these patient populations.
Methods: The data used for this study was collected from the TriNetX Network, which provided access to electronic medical records. We compared the data available in patients with CABG or POAF using AP and OC versus patients using AP only. The incidence of GIB in both these group were sought out. The number of these patients with GIB requiring transfusions, esophagogastroduodenoscopy (EGD) or interventional radiology embolization (IRE) were determined. The Odds ratio (OR) and Relative Risk (RR) in these groups with 95% Confidence Interval (CI) were calculated using statistical software. This was also examined for a p-value of < 0.05 significance.
Results: In CABG with POAF using AP and OC there was 301 with GIB events and 850 without any GIB. CABG with POAF using OC only 125 had GIB events while 1493 did not have any GIB events. Adverse events noted in the AP+ OC group was 26%, vs 7.7% patients in the AP group. The RR between the groups were 3.38 95% CI (2.78-4) with p-value < 0.0001. OR between the groups was 4.2; 95% CI (3.4-5.3). Number needed to harm (NNH) or cause GIB was 6; 95% CI (4.7- 6.4).
In the group with AP and OC 102 patients got blood transfusions, 59 received additional EGD and 10 required IRE eventually. The group with OC use, 44 patients got blood transfusions, 28 got EGD additionally and 10 required IRE eventually.
Discussion: The incidence of GIB as expected is more with AP and OC together in patients with CABG and POAF. NNH of 6 is high causing a GIB. Strengths of this study is that the data was obtained from multiple healthcare organizations. Limitations of this study is that an in-depth analysis of patient data and chronologic events was beyond the scope of this study. Detailed review after IRB approval is pending.
A need to stop, adjust or reconsider anticoagulation in patients with CABG and POAF is an important clinical decision that needs to be constantly addressed on subsequent visits between the clinician and the patient.

Figure: Acute GIB in post CABG/POAF patients on AP/OC
Disclosures:
Winnie Roy indicated no relevant financial relationships.
Umer Rizwan indicated no relevant financial relationships.
Mohamed Barakat indicated no relevant financial relationships.
Winnie Roy, MD, MPH, Umer Rizwan, MD, Mohamed Barakat, MD. P3463 - Acute GI Bleed Following CABG With Atrial Fibrillation on Antiplatelet and Anticoagulant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
