Tuesday Poster Session
Category: GI Bleeding
P3477 - Getting to the GIST: Straight to Surgery for Refractory GI Bleeding
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- ML
Marcia Leung, MD
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Marcia Leung, MD1, Lawrence Leung, MD, MPH1, Jeffrey Lee, MD, MPH2, Nizar A. Mukhtar, MD2, Lyle Shlager, MD1
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente San Francisco Medical Center, San Francisco, CA
Introduction: As gastrointestinal stromal tumors (GISTs) are rare they are often overlooked in the differential diagnosis for gastrointestinal bleeding. This case highlights the most common way that GISTs present clinically- via upper GI bleeding.
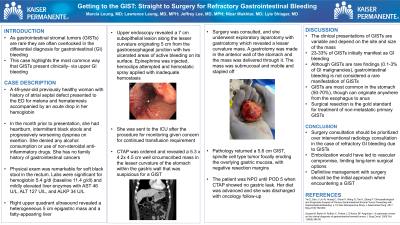
Case Description/Methods: A 49-year-old previously healthy woman was admitted for melena and hematemesis accompanied by acute anemia. In the past month, she had heartburn, intermittent black stools and worsening dyspnea on exertion. She denied any alcohol consumption or use of NSAIDs. She has no family history of gastrointestinal cancers. Physical exam was remarkable for soft black stool in the rectum. Labs were significant for hemoglobin 5.4 g/dl and mildly elevated liver enzymes with AST 46 U/L, ALT 127 U/L, and ALKP 34 U/L. Upper endoscopy revealed a 7 cm subepithelial lesion along the lesser curvature with two ulcerated areas of active bleeding on its surface. Epinephrine was injected, hemoclips attempted and hemostatic spray applied with inadequate hemostasis. She was sent to the ICU after the procedure for monitoring. CTAP revealed a 5.3 x 4.2x 4.5 cm well circumscribed mass in the lesser curvature of the stomach within the gastric wall that was suspicious for GIST. Surgery was consulted, and she underwent exploratory laparotomy which revealed a lesser curvature mass. A gastrotomy was made in the anterior wall of the stomach and the mass was delivered through it. The mass was submucosal and mobile and stapled off with a TA 90 mm stapler. Pathology returned a 5.6 cm gastrointestinal stromal tumor, spindle cell type tumor focally eroding the overlying gastric mucosa, with negative resection margins. The patient was NPO until POD 5 when CTAP showed no gastric leak. Her diet was advanced and she was discharged with oncology follow-up.
Discussion: 23-33% of GISTs initially manifest as GI bleeding. Although GISTs are rare (0.1-3% of GI malignancies), gastrointestinal bleeding should not be considered a rare manifestation of GISTs. Tumors are most common in the stomach (50-70%), though can originate anywhere from the esophagus to anus. Surgical resection is the gold standard for treatment of non-metastatic primary GISTs. As such, surgery consultation should be prioritized over interventional radiology consultation in the case of refractory gastrointestinal bleeding due to GISTs. Embolization would have led to vascular compromise, limiting long-term surgical options. Definitive management with surgery should be the initial approach when encountering a GIST.

Disclosures:
Marcia Leung, MD1, Lawrence Leung, MD, MPH1, Jeffrey Lee, MD, MPH2, Nizar A. Mukhtar, MD2, Lyle Shlager, MD1. P3477 - Getting to the GIST: Straight to Surgery for Refractory GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente San Francisco Medical Center, San Francisco, CA
Introduction: As gastrointestinal stromal tumors (GISTs) are rare they are often overlooked in the differential diagnosis for gastrointestinal bleeding. This case highlights the most common way that GISTs present clinically- via upper GI bleeding.
Case Description/Methods: A 49-year-old previously healthy woman was admitted for melena and hematemesis accompanied by acute anemia. In the past month, she had heartburn, intermittent black stools and worsening dyspnea on exertion. She denied any alcohol consumption or use of NSAIDs. She has no family history of gastrointestinal cancers. Physical exam was remarkable for soft black stool in the rectum. Labs were significant for hemoglobin 5.4 g/dl and mildly elevated liver enzymes with AST 46 U/L, ALT 127 U/L, and ALKP 34 U/L. Upper endoscopy revealed a 7 cm subepithelial lesion along the lesser curvature with two ulcerated areas of active bleeding on its surface. Epinephrine was injected, hemoclips attempted and hemostatic spray applied with inadequate hemostasis. She was sent to the ICU after the procedure for monitoring. CTAP revealed a 5.3 x 4.2x 4.5 cm well circumscribed mass in the lesser curvature of the stomach within the gastric wall that was suspicious for GIST. Surgery was consulted, and she underwent exploratory laparotomy which revealed a lesser curvature mass. A gastrotomy was made in the anterior wall of the stomach and the mass was delivered through it. The mass was submucosal and mobile and stapled off with a TA 90 mm stapler. Pathology returned a 5.6 cm gastrointestinal stromal tumor, spindle cell type tumor focally eroding the overlying gastric mucosa, with negative resection margins. The patient was NPO until POD 5 when CTAP showed no gastric leak. Her diet was advanced and she was discharged with oncology follow-up.
Discussion: 23-33% of GISTs initially manifest as GI bleeding. Although GISTs are rare (0.1-3% of GI malignancies), gastrointestinal bleeding should not be considered a rare manifestation of GISTs. Tumors are most common in the stomach (50-70%), though can originate anywhere from the esophagus to anus. Surgical resection is the gold standard for treatment of non-metastatic primary GISTs. As such, surgery consultation should be prioritized over interventional radiology consultation in the case of refractory gastrointestinal bleeding due to GISTs. Embolization would have led to vascular compromise, limiting long-term surgical options. Definitive management with surgery should be the initial approach when encountering a GIST.

Figure: Surgically resected GIST surface with ulcerations and deep erosions into underlying vessels
Disclosures:
Marcia Leung indicated no relevant financial relationships.
Lawrence Leung indicated no relevant financial relationships.
Jeffrey Lee indicated no relevant financial relationships.
Nizar Mukhtar indicated no relevant financial relationships.
Lyle Shlager indicated no relevant financial relationships.
Marcia Leung, MD1, Lawrence Leung, MD, MPH1, Jeffrey Lee, MD, MPH2, Nizar A. Mukhtar, MD2, Lyle Shlager, MD1. P3477 - Getting to the GIST: Straight to Surgery for Refractory GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
