Tuesday Poster Session
Category: GI Bleeding
P3485 - Complicated Management of a Bleeding Duodenal Amyloidoma in the Setting of Non-ST Segment Elevation Myocardial Infarction
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kevin Kadado, DO
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Kevin Kadado, DO, Abdul Rahman Akkawi, MD, Daly Al-Hadeethi, MD, Kyle Rowe, MD
University of Kansas School of Medicine, Wichita, KS
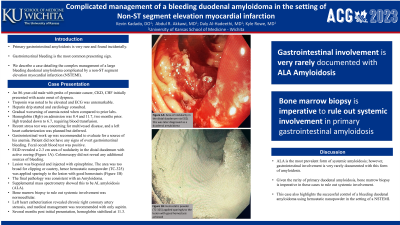
Introduction: Primary gastrointestinal amyloidosis is very rare and found incidentally. Albeit mostly being asymptomatic, gastrointestinal bleeding is the most common presenting sign. We describe a case detailing the complex management of a large bleeding duodenal amyloidoma complicated by a non-ST segment elevation myocardial infarction (NSTEMI).
Case Description/Methods: An 86-year-old male with past medical history of prostate cancer, chronic kidney disease, congestive heart failure initially presented with acute onset of dyspnea. On presentation, troponin was noted to be elevated and electrocardiogram was unremarkable, consistent with NSTEMI. He was started on a heparin drip and cardiology consulted. Further evaluation revealed that patient had gradual worsening of anemia when compared to prior labs. Hemoglobin (Hgb) on admission was 8.4 and 11.7, two months prior. Hgb trended down to 6.7, requiring blood transfusion. Recent stress test was concerning for multivessel disease, and a left heart catheterization was planned but deferred. Gastrointestinal work up was recommended to evaluate for a source of his anemia. Patient did not have any signs of overt gastrointestinal bleeding. Fecal occult blood test was positive, however, and esophagogastroduodenoscopy (EGD) and colonoscopy were performed. EGD revealed a 2-3 cm area of nodularity in the distal duodenum with active oozing (Figure 1A). This lesion was biopsied and injected with epinephrine. The area was too broad for clipping or cautery, hence hemostatic nanopowder (TC-325) was applied sparingly to the lesion with good hemostasis. The final pathology was consistent with an amyloidoma. Supplemental mass spectrometry showed this to be AL amyloidosis (ALA).Colonoscopy did not reveal any additional sources of bleeding. Bone marrow biopsy to rule out systemic involvement was normocellular. Left heart catheterization revealed chronic right coronary artery stenosis, and medical management was recommended with only aspirin. Several months post initial presentation, hemoglobin stabilized at 11.3.
Discussion: ALA is the most prevalent form of systemic amyloidosis; however, gastrointestinal involvement is very rarely documented with this form of amyloidosis. Given the rarity of primary duodenal amyloidosis, bone marrow biopsy is imperative in these cases to rule out systemic involvement. This case highlights the successful control of a bleeding duodenal amyloidoma using hemostatic nanopowder in the setting of a NSTEMI.
Disclosures:
Kevin Kadado, DO, Abdul Rahman Akkawi, MD, Daly Al-Hadeethi, MD, Kyle Rowe, MD. P3485 - Complicated Management of a Bleeding Duodenal Amyloidoma in the Setting of Non-ST Segment Elevation Myocardial Infarction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kansas School of Medicine, Wichita, KS
Introduction: Primary gastrointestinal amyloidosis is very rare and found incidentally. Albeit mostly being asymptomatic, gastrointestinal bleeding is the most common presenting sign. We describe a case detailing the complex management of a large bleeding duodenal amyloidoma complicated by a non-ST segment elevation myocardial infarction (NSTEMI).
Case Description/Methods: An 86-year-old male with past medical history of prostate cancer, chronic kidney disease, congestive heart failure initially presented with acute onset of dyspnea. On presentation, troponin was noted to be elevated and electrocardiogram was unremarkable, consistent with NSTEMI. He was started on a heparin drip and cardiology consulted. Further evaluation revealed that patient had gradual worsening of anemia when compared to prior labs. Hemoglobin (Hgb) on admission was 8.4 and 11.7, two months prior. Hgb trended down to 6.7, requiring blood transfusion. Recent stress test was concerning for multivessel disease, and a left heart catheterization was planned but deferred. Gastrointestinal work up was recommended to evaluate for a source of his anemia. Patient did not have any signs of overt gastrointestinal bleeding. Fecal occult blood test was positive, however, and esophagogastroduodenoscopy (EGD) and colonoscopy were performed. EGD revealed a 2-3 cm area of nodularity in the distal duodenum with active oozing (Figure 1A). This lesion was biopsied and injected with epinephrine. The area was too broad for clipping or cautery, hence hemostatic nanopowder (TC-325) was applied sparingly to the lesion with good hemostasis. The final pathology was consistent with an amyloidoma. Supplemental mass spectrometry showed this to be AL amyloidosis (ALA).Colonoscopy did not reveal any additional sources of bleeding. Bone marrow biopsy to rule out systemic involvement was normocellular. Left heart catheterization revealed chronic right coronary artery stenosis, and medical management was recommended with only aspirin. Several months post initial presentation, hemoglobin stabilized at 11.3.
Discussion: ALA is the most prevalent form of systemic amyloidosis; however, gastrointestinal involvement is very rarely documented with this form of amyloidosis. Given the rarity of primary duodenal amyloidosis, bone marrow biopsy is imperative in these cases to rule out systemic involvement. This case highlights the successful control of a bleeding duodenal amyloidoma using hemostatic nanopowder in the setting of a NSTEMI.
Disclosures:
Kevin Kadado indicated no relevant financial relationships.
Abdul Rahman Akkawi indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
Kevin Kadado, DO, Abdul Rahman Akkawi, MD, Daly Al-Hadeethi, MD, Kyle Rowe, MD. P3485 - Complicated Management of a Bleeding Duodenal Amyloidoma in the Setting of Non-ST Segment Elevation Myocardial Infarction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
