Tuesday Poster Session
Category: GI Bleeding
P3495 - An Unexpected Discovery of Aortoenteric Fistula in the Absence of Active Bleeding
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Rabih Ghazi, MD
Cooper University Hospital at Cooper Medical School at Rowan University
Philadelphia, Pennsylvania
Presenting Author(s)
Rabih Ghazi, MD1, Rita Auro, MD2, Rachel Frank, MD2
1Cooper University Hospital at Cooper Medical School at Rowan University, Philadelphia, PA; 2Cooper University Hospital, Camden, NJ
Introduction: Aortoenteric fistula (AEF) is a rare, life-threatening condition typically found in patients with a history of aortic aneurysm or intervention. The most common symptom is massive gastrointestinal (GI) bleeding. We present a case of a patient with an extensive vascular history who had an AEF discovered during an esophagogastroduodenoscopy (EGD) without any bleeding.
Case Description/Methods: A 58-year-old male with a history of abdominal aortic aneurysm repair and peripheral artery disease with multiple vascular procedures, including aorto-uni-iliac bypass requiring thrombectomy with stent grafting 1 year prior, presented to the gastroenterology office for evaluation of generalized abdominal pain and intermittent dark stools, and weight loss. EGD revealed a polypoid and sessile non-bleeding mass in the duodenum, a few centimeters distal to the papilla. Biopsy showed mucosal ulceration and granulation tissue in the mucosa without dysplasia or carcinoma. A repeat EGD performed 2 weeks later for mass resection did not visualize the mass but revealed a 20mm AEF in the third part of the duodenum, with the aortic graft visible. Inflammatory changes were noted but there was no active bleeding. He was recommended to seek urgent evaluation by vascular surgery. Upon hospital arrival, hemoglobin was 10 g/dl. CT angiography (CTA) revealed no active bleeding but did show close proximity of the transverse duodenum to the proximal aortic graft, with some gas observed between the two. He underwent an exploratory laparotomy with small bowel resection and anastomosis, and a left axillary artery to left superficial femoral artery bypass.
Discussion: Extra vigilance is crucial for patients with a history of aortic aneurysm or intervention who exhibit GI bleeding, as these cases can present with hemodynamic instability and can be life-threatening. Typically, the initial diagnosis is made via CTA. This case is unique in that an AEF was identified during an EGD performed to evaluate abdominal pain, weight loss, and melena. The duodenal mass was likely a result of the aorta protruding into the duodenum. A follow-up EGD revealed a fistula with an aortic graft extending through the duodenum, which likely acted as a tamponade. The patient was able to receive appropriate intervention without hemodynamic compromise. This rare case of AEF highlights the importance of maintaining a low threshold for workup when evaluating GI symptoms in this patient population, particularly in those found have with duodenal polyps or mass.

Disclosures:
Rabih Ghazi, MD1, Rita Auro, MD2, Rachel Frank, MD2. P3495 - An Unexpected Discovery of Aortoenteric Fistula in the Absence of Active Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cooper University Hospital at Cooper Medical School at Rowan University, Philadelphia, PA; 2Cooper University Hospital, Camden, NJ
Introduction: Aortoenteric fistula (AEF) is a rare, life-threatening condition typically found in patients with a history of aortic aneurysm or intervention. The most common symptom is massive gastrointestinal (GI) bleeding. We present a case of a patient with an extensive vascular history who had an AEF discovered during an esophagogastroduodenoscopy (EGD) without any bleeding.
Case Description/Methods: A 58-year-old male with a history of abdominal aortic aneurysm repair and peripheral artery disease with multiple vascular procedures, including aorto-uni-iliac bypass requiring thrombectomy with stent grafting 1 year prior, presented to the gastroenterology office for evaluation of generalized abdominal pain and intermittent dark stools, and weight loss. EGD revealed a polypoid and sessile non-bleeding mass in the duodenum, a few centimeters distal to the papilla. Biopsy showed mucosal ulceration and granulation tissue in the mucosa without dysplasia or carcinoma. A repeat EGD performed 2 weeks later for mass resection did not visualize the mass but revealed a 20mm AEF in the third part of the duodenum, with the aortic graft visible. Inflammatory changes were noted but there was no active bleeding. He was recommended to seek urgent evaluation by vascular surgery. Upon hospital arrival, hemoglobin was 10 g/dl. CT angiography (CTA) revealed no active bleeding but did show close proximity of the transverse duodenum to the proximal aortic graft, with some gas observed between the two. He underwent an exploratory laparotomy with small bowel resection and anastomosis, and a left axillary artery to left superficial femoral artery bypass.
Discussion: Extra vigilance is crucial for patients with a history of aortic aneurysm or intervention who exhibit GI bleeding, as these cases can present with hemodynamic instability and can be life-threatening. Typically, the initial diagnosis is made via CTA. This case is unique in that an AEF was identified during an EGD performed to evaluate abdominal pain, weight loss, and melena. The duodenal mass was likely a result of the aorta protruding into the duodenum. A follow-up EGD revealed a fistula with an aortic graft extending through the duodenum, which likely acted as a tamponade. The patient was able to receive appropriate intervention without hemodynamic compromise. This rare case of AEF highlights the importance of maintaining a low threshold for workup when evaluating GI symptoms in this patient population, particularly in those found have with duodenal polyps or mass.

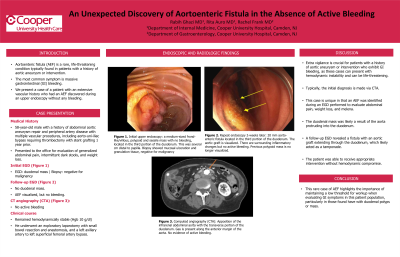
Figure: (A) Initial upper endoscopy: a medium-sized frond-like/villous, polypoid and sessile mass with no bleeding, located in the third portion of the duodenum. This was several cm distal to papilla.
(B) Repeat endoscopy 2-weeks later: 20 mm aorto-enteric fistula located in the third portion of the duodenum. The aortic graft is visualized. There are surrounding inflammatory changes but no active bleeding. Previous polypoid mass is no longer visualized.
(C) Computed angiography (CTA): Apposition of the infrarenal abdominal aorta with the transverse portion of the duodenum. Gas is present along the anterior margin of the aorta. No evidence of active bleeding.
(B) Repeat endoscopy 2-weeks later: 20 mm aorto-enteric fistula located in the third portion of the duodenum. The aortic graft is visualized. There are surrounding inflammatory changes but no active bleeding. Previous polypoid mass is no longer visualized.
(C) Computed angiography (CTA): Apposition of the infrarenal abdominal aorta with the transverse portion of the duodenum. Gas is present along the anterior margin of the aorta. No evidence of active bleeding.
Disclosures:
Rabih Ghazi indicated no relevant financial relationships.
Rita Auro indicated no relevant financial relationships.
Rachel Frank indicated no relevant financial relationships.
Rabih Ghazi, MD1, Rita Auro, MD2, Rachel Frank, MD2. P3495 - An Unexpected Discovery of Aortoenteric Fistula in the Absence of Active Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
