Tuesday Poster Session
Category: GI Bleeding
P3518 - The Impact of Novel Endoscopic Treatment Modalities on Patient Outcome in Severe Upper GI Bleeding: A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AP
Amulya Penmetsa, MD
University of Rochester Medical Center
Rochester, New York
Presenting Author(s)
Amulya Penmetsa, MD1, Julia Burke, PA-C1, Peter Fields, MD1, Nicholas Bartell, MD1, Brandon Sprung, MD1, Vivek Kaul, MD, FACG2
1University of Rochester Medical Center, Rochester, NY; 2University of Rochester, Rochester, NY
Introduction: Non-variceal upper gastrointestinal (GI) bleeding remains a common clinical issue resulting in hospital admissions, high cost and morbidity. Novel technologies have emerged that help with endoscopic salvage in patients with severe GI bleeding refractory to traditional interventions or when these are not feasible. We present a case to highlight the impact of this new paradigm in endoscopy.
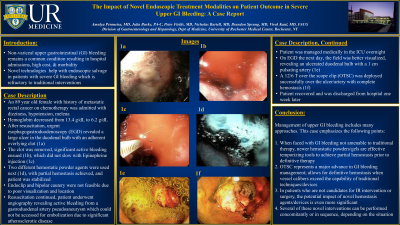
Case Description/Methods: An 89 year old female with history of metastatic rectal cancer on chemotherapy, renal failure, and coronary artery disease was admitted with dizziness, hypotension, melena and hemoglobin drop to 6.2 g/dL from baseline 13.4 g/dL. After resuscitation, urgent esophagogastroduodenoscopy (EGD) revealed a large ulcer in the duodenal bulb with an adherent overlying clot (1a). The clot was removed, significant active bleeding ensued (1b). Epinephrine injection did not slow bleeding (1c). Two different hemostatic powder agents were used next (1d), with only partial hemostasis achieved. Endoclip and bipolar cautery were not feasible due to poor visualization and location. Resuscitation continued and the patient underwent angiography revealing active bleeding from a gastroduodenal artery pseudoaneurysm which could not be accessed for embolization due to significant atherosclerotic disease. The patient was managed medically in intensive care. Repeat EGD the next day revealed an ulcerated duodenal bulb with a 1 cm pulsating artery (1e). A 12/6 T over the scope clip (OTSC) was deployed successfully over the ulcer/artery with complete hemostasis (1f). The patient stabilized and was discharged from the hospital one week later.
Discussion: Management of upper GI bleeding includes many approaches. This case emphasizes the following points:
1. When faced with GI bleeding not amenable to traditional therapy, newer hemostatic powders/gels are effective temporizing tools to achieve partial hemostasis prior to definitive therapy.
2. OTSC represents a major advance in GI bleeding management as it allows for definitive hemostasis when vessel calibers exceed the capability of traditional techniques or devices.
3. In patients who are not candidates for IR intervention or surgery, the potential impact of novel hemostasis agents/devices is even more significant.
4. Several of these novel interventions can be performed concomitantly or in sequence, depending on the situation.
5. Endoscopists should be familiar with these novel techniques and consider these interventions when managing severe GI bleeding cases.

Disclosures:
Amulya Penmetsa, MD1, Julia Burke, PA-C1, Peter Fields, MD1, Nicholas Bartell, MD1, Brandon Sprung, MD1, Vivek Kaul, MD, FACG2. P3518 - The Impact of Novel Endoscopic Treatment Modalities on Patient Outcome in Severe Upper GI Bleeding: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Rochester Medical Center, Rochester, NY; 2University of Rochester, Rochester, NY
Introduction: Non-variceal upper gastrointestinal (GI) bleeding remains a common clinical issue resulting in hospital admissions, high cost and morbidity. Novel technologies have emerged that help with endoscopic salvage in patients with severe GI bleeding refractory to traditional interventions or when these are not feasible. We present a case to highlight the impact of this new paradigm in endoscopy.
Case Description/Methods: An 89 year old female with history of metastatic rectal cancer on chemotherapy, renal failure, and coronary artery disease was admitted with dizziness, hypotension, melena and hemoglobin drop to 6.2 g/dL from baseline 13.4 g/dL. After resuscitation, urgent esophagogastroduodenoscopy (EGD) revealed a large ulcer in the duodenal bulb with an adherent overlying clot (1a). The clot was removed, significant active bleeding ensued (1b). Epinephrine injection did not slow bleeding (1c). Two different hemostatic powder agents were used next (1d), with only partial hemostasis achieved. Endoclip and bipolar cautery were not feasible due to poor visualization and location. Resuscitation continued and the patient underwent angiography revealing active bleeding from a gastroduodenal artery pseudoaneurysm which could not be accessed for embolization due to significant atherosclerotic disease. The patient was managed medically in intensive care. Repeat EGD the next day revealed an ulcerated duodenal bulb with a 1 cm pulsating artery (1e). A 12/6 T over the scope clip (OTSC) was deployed successfully over the ulcer/artery with complete hemostasis (1f). The patient stabilized and was discharged from the hospital one week later.
Discussion: Management of upper GI bleeding includes many approaches. This case emphasizes the following points:
1. When faced with GI bleeding not amenable to traditional therapy, newer hemostatic powders/gels are effective temporizing tools to achieve partial hemostasis prior to definitive therapy.
2. OTSC represents a major advance in GI bleeding management as it allows for definitive hemostasis when vessel calibers exceed the capability of traditional techniques or devices.
3. In patients who are not candidates for IR intervention or surgery, the potential impact of novel hemostasis agents/devices is even more significant.
4. Several of these novel interventions can be performed concomitantly or in sequence, depending on the situation.
5. Endoscopists should be familiar with these novel techniques and consider these interventions when managing severe GI bleeding cases.

Figure: Endoscopic images demonstrating actively bleeding ulcer with various interventions
1a: Large duodenal bulb ulcer with overlying adherent clot
1b: Significant active bleeding after removal of clot
1c: Injection of epinephrine with no improvement
1d: Hemostatic powder agents x 2 application with partial hemostasis
1e: Large pulsating artery within the duodenal bulb ulcer
1f: Successful deployment of OTSC with complete hemostasis
1a: Large duodenal bulb ulcer with overlying adherent clot
1b: Significant active bleeding after removal of clot
1c: Injection of epinephrine with no improvement
1d: Hemostatic powder agents x 2 application with partial hemostasis
1e: Large pulsating artery within the duodenal bulb ulcer
1f: Successful deployment of OTSC with complete hemostasis
Disclosures:
Amulya Penmetsa indicated no relevant financial relationships.
Julia Burke indicated no relevant financial relationships.
Peter Fields indicated no relevant financial relationships.
Nicholas Bartell indicated no relevant financial relationships.
Brandon Sprung indicated no relevant financial relationships.
Vivek Kaul: CASTLE BIOSCIENCES – Consultant. CDX DIAGNOSTICS – Consultant. COOK MEDICAL – Consultant. MOTUS GI – Consultant. STERIS – Consultant.
Amulya Penmetsa, MD1, Julia Burke, PA-C1, Peter Fields, MD1, Nicholas Bartell, MD1, Brandon Sprung, MD1, Vivek Kaul, MD, FACG2. P3518 - The Impact of Novel Endoscopic Treatment Modalities on Patient Outcome in Severe Upper GI Bleeding: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
