Tuesday Poster Session
Category: IBD
P3552 - Efficacy of Vedolizumab Therapy in Patients With Perianal Crohn’s Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Scott Manski, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Scott Manski, MD1, Chelsea Edirisuriya, MD1, Joseph Fabrizio, BS2, Vincent Dioguardi, MD1, Hema K.. Gandhi, MPH2, Raina Shivashankar, MD, FACG1
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Thomas Jefferson University, Philadelphia, PA
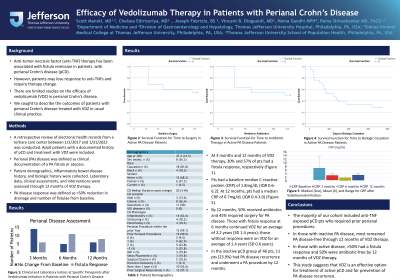
Introduction: Anti-tumor necrosis factor (anti-TNF) therapy has been associated with fistula remission in patients (pts) with perianal Crohn’s disease (pCD). However, pts may lose response to anti-TNFs and require therapy change. There are limited studies on the efficacy of vedolizumab (VDZ) in pCD. We sought to describe the outcomes of pts with pCD treated with VDZ in usual clinical practice.
Methods: A retrospective review of electronic health records from a tertiary care center between 1/1/2017 and 1/31/2022 was conducted. Adult pts with a documented history of pCD and treatment with VDZ were included. Perianal (PA) disease was defined as clinical documentation of a PA fistula or abscess. Patient demographics, inflammatory bowel disease history, and biologic history were collected. Laboratory data, clinical assessments, and interventions were assessed through 12 months of VDZ therapy. PA disease response was defined as >50% reduction in drainage and number of fistulae from baseline.
Results: 68 pts with pCD treated with VDZ were identified. Of those, 22 pts had active PA lesions at the time of VDZ initiation. In this subgroup, the average age was 47.4 years (SD: 14.5 years); CD median duration was 20 years (range: 3-45 years). 36% of pts were male. 86% of pts were previously treated with infliximab and 82% treated with adalimumab. 90% of pts had a history of a PA procedure with 48% having at least 2 prior PA procedures. At 3 months and 12 months of VDZ therapy, 30% and 57% of pts had a fistula response, respectively (Table 1). Pts had a baseline median C-reactive protein (CRP) of 1.8mg/dL (IQR 0.6-6.2). At 12 months, pts had a median CRP of 0.7mg/dL (IQR 0.4-3.0). By 12 months, 50% received antibiotics and 45% required surgery for PA disease. Those with fistula response at 6 months continued VDZ for an average of 2.2 years (SD 1.4 years); those without response were on VDZ for an average of 1.4 years (SD 0.6 years). In the inactive pCD group of 46 pts, 11 pts (23.9%) had PA disease recurrence and underwent a PA procedure by 12 months.
Discussion: The majority of our cohort included anti-TNF exposed pCD pts who required prior perianal procedures. In those with inactive PA disease, most remained PA disease-free through 12 months of VDZ therapy. In those with active disease, >50% had a fistula response and 50% were antibiotic-free by 12 months of VDZ therapy. This study suggests that VDZ is an effective option for treatment of active pCD and for prevention of PA disease recurrence.
Disclosures:
Scott Manski, MD1, Chelsea Edirisuriya, MD1, Joseph Fabrizio, BS2, Vincent Dioguardi, MD1, Hema K.. Gandhi, MPH2, Raina Shivashankar, MD, FACG1. P3552 - Efficacy of Vedolizumab Therapy in Patients With Perianal Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Thomas Jefferson University, Philadelphia, PA
Introduction: Anti-tumor necrosis factor (anti-TNF) therapy has been associated with fistula remission in patients (pts) with perianal Crohn’s disease (pCD). However, pts may lose response to anti-TNFs and require therapy change. There are limited studies on the efficacy of vedolizumab (VDZ) in pCD. We sought to describe the outcomes of pts with pCD treated with VDZ in usual clinical practice.
Methods: A retrospective review of electronic health records from a tertiary care center between 1/1/2017 and 1/31/2022 was conducted. Adult pts with a documented history of pCD and treatment with VDZ were included. Perianal (PA) disease was defined as clinical documentation of a PA fistula or abscess. Patient demographics, inflammatory bowel disease history, and biologic history were collected. Laboratory data, clinical assessments, and interventions were assessed through 12 months of VDZ therapy. PA disease response was defined as >50% reduction in drainage and number of fistulae from baseline.
Results: 68 pts with pCD treated with VDZ were identified. Of those, 22 pts had active PA lesions at the time of VDZ initiation. In this subgroup, the average age was 47.4 years (SD: 14.5 years); CD median duration was 20 years (range: 3-45 years). 36% of pts were male. 86% of pts were previously treated with infliximab and 82% treated with adalimumab. 90% of pts had a history of a PA procedure with 48% having at least 2 prior PA procedures. At 3 months and 12 months of VDZ therapy, 30% and 57% of pts had a fistula response, respectively (Table 1). Pts had a baseline median C-reactive protein (CRP) of 1.8mg/dL (IQR 0.6-6.2). At 12 months, pts had a median CRP of 0.7mg/dL (IQR 0.4-3.0). By 12 months, 50% received antibiotics and 45% required surgery for PA disease. Those with fistula response at 6 months continued VDZ for an average of 2.2 years (SD 1.4 years); those without response were on VDZ for an average of 1.4 years (SD 0.6 years). In the inactive pCD group of 46 pts, 11 pts (23.9%) had PA disease recurrence and underwent a PA procedure by 12 months.
Discussion: The majority of our cohort included anti-TNF exposed pCD pts who required prior perianal procedures. In those with inactive PA disease, most remained PA disease-free through 12 months of VDZ therapy. In those with active disease, >50% had a fistula response and 50% were antibiotic-free by 12 months of VDZ therapy. This study suggests that VDZ is an effective option for treatment of active pCD and for prevention of PA disease recurrence.
Disclosures:
Scott Manski indicated no relevant financial relationships.
Chelsea Edirisuriya indicated no relevant financial relationships.
Joseph Fabrizio indicated no relevant financial relationships.
Vincent Dioguardi indicated no relevant financial relationships.
Hema Gandhi indicated no relevant financial relationships.
Raina Shivashankar: Abbvie – Grant/Research Support, Speakers Bureau. Bristol Meyers Squibb – Speakers Bureau. Janssen – Advisory Committee/Board Member, Grant/Research Support.
Scott Manski, MD1, Chelsea Edirisuriya, MD1, Joseph Fabrizio, BS2, Vincent Dioguardi, MD1, Hema K.. Gandhi, MPH2, Raina Shivashankar, MD, FACG1. P3552 - Efficacy of Vedolizumab Therapy in Patients With Perianal Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
