Tuesday Poster Session
Category: IBD
P3575 - Unveiling the Link Between Ulcerative Colitis and Gastroparesis: A Population-Based Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Xiaoliang Wang, MD, PhD
Marshall University School of Medicine
Huntington, WV
Presenting Author(s)
Xiaoliang Wang, MD, PhD1, Michael Kurin, MD2, Marc Landsman, MD3, Braden Kuo, MD4, Jiayan Wang, MD, PhD1, Gengqing Song, MD3
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth, Cleveland, OH; 3MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH; 4Massachusetts General Hospital, Boston, MA
Introduction: Ulcerative colitis (UC) is a chronic immune disorder characterized by diarrhea, abdominal pain, bloody or purulent stools, weight loss, and sometimes unexplained nausea, vomiting, or epigastric discomfort. Whether these symptoms are related to UC or may be caused by separate upper GI disorders remains unknown. We investigated whether there is an increased prevalence of gastroparesis in patients with UC.
Methods: We conducted an analysis using the Population-based National Inpatient Sample (NIS) dataset, which included 7,159,694 patients. We included patients diagnosed with gastroparesis with or without UC. We also performed a subgroup analysis of UC subtypes based on involved colonic segments. We adjusted for potential risk factors that could impact the prevalence of gastroparesis and UC, such as age, gender, race, type 2 DM, smoking history. Our primary aim was to determine gastroparesis prevalence and odds ratio in UC patients, while also examining the co-existence of gastroesophageal reflux disease (GERD). Categorical variable differences between groups were assessed through bivariate analyses using chi-squared or Fisher exact tests.
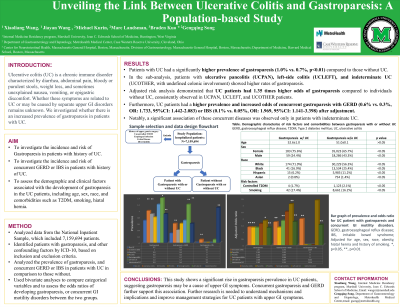
Results: Patients with UC had a significantly higher prevalence of gastroparesis (1.0% vs. 0.7%, p< 0.01) compared to those without UC, which was associate with high risk of having gastroparesis (OR: 1.35, 95% CI: 1.157-1.494). In the sub-analysis, patients with ulcerative pancolitis (UCPAN), left-side colitis (UCLEFT), and indeterminate UC (UCOTHER, with undefined colonic involvement) showed higher rates of gastroparesis. Adjusted risk analysis demonstrated that UC patients had 1.35 times higher odds of gastroparesis compared to individuals without UC, consistently observed in UCPAN, UCLEFT, and UCOTHER patients. Furthermore, UC patients had a higher prevalence and increased odds of concurrent gastroparesis with GERD (0.6% vs. 0.3%, OR: 1.733, 95%CI: 1.442-2.083) or IBS (0.1% vs. 0.05%, OR: 1.969, 95%CI: 1.141-3.398) after adjustment. Notably, a significant association of these concurrent diseases was observed only in patients with UCOTHER.
Discussion: This study shows a significant rise in gastroparesis prevalence in UC patients, suggesting gastroparesis may be a cause of upper GI symptoms. Concurrent gastroparesis and GERD further support this association. Further research is needed to understand mechanisms and implications and improve management strategies for UC patients with upper GI symptoms.

Disclosures:
Xiaoliang Wang, MD, PhD1, Michael Kurin, MD2, Marc Landsman, MD3, Braden Kuo, MD4, Jiayan Wang, MD, PhD1, Gengqing Song, MD3. P3575 - Unveiling the Link Between Ulcerative Colitis and Gastroparesis: A Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth, Cleveland, OH; 3MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH; 4Massachusetts General Hospital, Boston, MA
Introduction: Ulcerative colitis (UC) is a chronic immune disorder characterized by diarrhea, abdominal pain, bloody or purulent stools, weight loss, and sometimes unexplained nausea, vomiting, or epigastric discomfort. Whether these symptoms are related to UC or may be caused by separate upper GI disorders remains unknown. We investigated whether there is an increased prevalence of gastroparesis in patients with UC.
Methods: We conducted an analysis using the Population-based National Inpatient Sample (NIS) dataset, which included 7,159,694 patients. We included patients diagnosed with gastroparesis with or without UC. We also performed a subgroup analysis of UC subtypes based on involved colonic segments. We adjusted for potential risk factors that could impact the prevalence of gastroparesis and UC, such as age, gender, race, type 2 DM, smoking history. Our primary aim was to determine gastroparesis prevalence and odds ratio in UC patients, while also examining the co-existence of gastroesophageal reflux disease (GERD). Categorical variable differences between groups were assessed through bivariate analyses using chi-squared or Fisher exact tests.
Results: Patients with UC had a significantly higher prevalence of gastroparesis (1.0% vs. 0.7%, p< 0.01) compared to those without UC, which was associate with high risk of having gastroparesis (OR: 1.35, 95% CI: 1.157-1.494). In the sub-analysis, patients with ulcerative pancolitis (UCPAN), left-side colitis (UCLEFT), and indeterminate UC (UCOTHER, with undefined colonic involvement) showed higher rates of gastroparesis. Adjusted risk analysis demonstrated that UC patients had 1.35 times higher odds of gastroparesis compared to individuals without UC, consistently observed in UCPAN, UCLEFT, and UCOTHER patients. Furthermore, UC patients had a higher prevalence and increased odds of concurrent gastroparesis with GERD (0.6% vs. 0.3%, OR: 1.733, 95%CI: 1.442-2.083) or IBS (0.1% vs. 0.05%, OR: 1.969, 95%CI: 1.141-3.398) after adjustment. Notably, a significant association of these concurrent diseases was observed only in patients with UCOTHER.
Discussion: This study shows a significant rise in gastroparesis prevalence in UC patients, suggesting gastroparesis may be a cause of upper GI symptoms. Concurrent gastroparesis and GERD further support this association. Further research is needed to understand mechanisms and implications and improve management strategies for UC patients with upper GI symptoms.

Figure: Figure A, Demographic characterize, risk factors and comorbidities between UC with and without Gastroparesis. B, Prevalence and odds ratio of gastroparesis and concurrent GI motility disorder in patients with all types of UC. C. Bar graph of prevalence and odds ratio of gastroparesis and concurrent GI motility disorder in patients with All type of UC. GERD, gastroesophageal reflux disease; UC, ulcerative colitis, UCPAN, ulcerative pancolitis; UCRPOC, ulcerative proctitis; UCRESCSIG, ulcerative rectosigmoiditis; UCLEFT, left-side colitis; UCOTHER, indetermined UC; OR, odds ratio *, p<0.05; **, p<0.01
Disclosures:
Xiaoliang Wang indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Marc Landsman indicated no relevant financial relationships.
Braden Kuo indicated no relevant financial relationships.
Jiayan Wang indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Xiaoliang Wang, MD, PhD1, Michael Kurin, MD2, Marc Landsman, MD3, Braden Kuo, MD4, Jiayan Wang, MD, PhD1, Gengqing Song, MD3. P3575 - Unveiling the Link Between Ulcerative Colitis and Gastroparesis: A Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

