Monday Poster Session
Category: Biliary/Pancreas
P1429 - Post Endoscopic Retrograde Cholangiopancreatography Pancreatitis Prophylaxis: All, Some, or None?
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- DB
David S. Braun, MD
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
David S. Braun, MD, Prashant S. Kedia, MD, David Lee, MD, Paul Tarnasky, MD
Methodist Dallas Medical Center, Dallas, TX
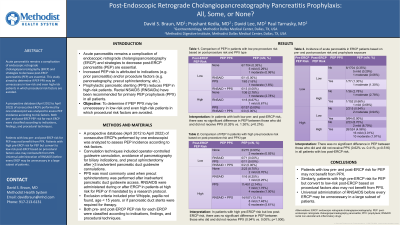
Introduction: Acute pancreatitis remains a complication of endoscopic retrograde cholangiopancreatography (ERCP) and strategies to decrease post-ERCP pancreatitis (PEP) are essential. Increased PEP risk is attributed to indications (e.g. prior pancreatitis) and/or procedure factors (e.g. pancreatography). Prophylactic pancreatic stenting (PPS) reduces PEP in high-risk patients. Rectal NSAIDS (RNSAIDs) have been recommended for primary PEP prophylaxis (PPX) in all patients; most experts recommend that RNSAIDs be administered before ERCP or at the time of cannulation attempts. The aim of this study was to determine if PEP PPX may be unnecessary in low-risk and even high-risk patients in which procedural risk factors are avoided.
Methods: A prospective database (April 2012 to April 2022) of consecutive ERCPs performed by one endoscopist was analyzed to assess PEP incidence according to risk factors. Cannulation techniques included operator-controlled guidewire cannulation, avoidance of pancreatography for biliary indications, and precut sphincterotomy after >3 inadvertent pancreatic duct guidewire cannulations. PPS was most commonly used when precut sphincterotomy was performed after inadvertent pancreatic duct guidewire access. RNSAIDS were administered during or after ERCP in patients at high risk for PEP or if mandated by a research protocol. Exclusion criteria included prior Whipple, papilla not found, age < 15 years, or if pancreatic duct stents were required for therapy. Both pre- and post-ERCP PEP risk for each ERCP were classified according to indications, findings, and procedural techniques.
Results: A total of 3132 patients (female: 58.1%; median age: 59) were included in this study. In patients with both low pre- and post-ERCP risk, there was no significant difference in PEP between those who did and did not receive PPX (0.35% vs. 1.30%; p=0.216). In patients with high pre-ERCP risk but low post-ERCP risk, there was no significant difference in PEP between those who did and did not receive PPX (0.94% vs. 0.00%; p=1.000). There was no significant difference in PEP between those who did and did not receive PPX (0.62% vs. 0.41%; p=0.516) in all patients with low post-ERCP risk.
Discussion: Patients with low pre- and post-ERCP risk for PEP may not benefit from PPX. Patients with high pre-ERCP risk for PEP but convert to low-risk post-ERCP based on procedural factors also may not benefit from PPX. Universal administration of RNSAIDS before every ERCP may be unnecessary in a large subset of patients.
Disclosures:
David S. Braun, MD, Prashant S. Kedia, MD, David Lee, MD, Paul Tarnasky, MD. P1429 - Post Endoscopic Retrograde Cholangiopancreatography Pancreatitis Prophylaxis: All, Some, or None?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Methodist Dallas Medical Center, Dallas, TX
Introduction: Acute pancreatitis remains a complication of endoscopic retrograde cholangiopancreatography (ERCP) and strategies to decrease post-ERCP pancreatitis (PEP) are essential. Increased PEP risk is attributed to indications (e.g. prior pancreatitis) and/or procedure factors (e.g. pancreatography). Prophylactic pancreatic stenting (PPS) reduces PEP in high-risk patients. Rectal NSAIDS (RNSAIDs) have been recommended for primary PEP prophylaxis (PPX) in all patients; most experts recommend that RNSAIDs be administered before ERCP or at the time of cannulation attempts. The aim of this study was to determine if PEP PPX may be unnecessary in low-risk and even high-risk patients in which procedural risk factors are avoided.
Methods: A prospective database (April 2012 to April 2022) of consecutive ERCPs performed by one endoscopist was analyzed to assess PEP incidence according to risk factors. Cannulation techniques included operator-controlled guidewire cannulation, avoidance of pancreatography for biliary indications, and precut sphincterotomy after >3 inadvertent pancreatic duct guidewire cannulations. PPS was most commonly used when precut sphincterotomy was performed after inadvertent pancreatic duct guidewire access. RNSAIDS were administered during or after ERCP in patients at high risk for PEP or if mandated by a research protocol. Exclusion criteria included prior Whipple, papilla not found, age < 15 years, or if pancreatic duct stents were required for therapy. Both pre- and post-ERCP PEP risk for each ERCP were classified according to indications, findings, and procedural techniques.
Results: A total of 3132 patients (female: 58.1%; median age: 59) were included in this study. In patients with both low pre- and post-ERCP risk, there was no significant difference in PEP between those who did and did not receive PPX (0.35% vs. 1.30%; p=0.216). In patients with high pre-ERCP risk but low post-ERCP risk, there was no significant difference in PEP between those who did and did not receive PPX (0.94% vs. 0.00%; p=1.000). There was no significant difference in PEP between those who did and did not receive PPX (0.62% vs. 0.41%; p=0.516) in all patients with low post-ERCP risk.
Discussion: Patients with low pre- and post-ERCP risk for PEP may not benefit from PPX. Patients with high pre-ERCP risk for PEP but convert to low-risk post-ERCP based on procedural factors also may not benefit from PPX. Universal administration of RNSAIDS before every ERCP may be unnecessary in a large subset of patients.
Disclosures:
David Braun indicated no relevant financial relationships.
Prashant Kedia: Boston Scientific – Consultant. Medtronic – Consultant. Olympus – Consultant.
David Lee indicated no relevant financial relationships.
Paul Tarnasky indicated no relevant financial relationships.
David S. Braun, MD, Prashant S. Kedia, MD, David Lee, MD, Paul Tarnasky, MD. P1429 - Post Endoscopic Retrograde Cholangiopancreatography Pancreatitis Prophylaxis: All, Some, or None?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
