Monday Poster Session
Category: Biliary/Pancreas
P1436 - Association Between Aspirin Use and Acute Pancreatitis in Patients With Alcohol Use Disorder
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- PB
Praneeth Bandaru, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Vijay Gayam, MD1, Vishnu Poojitha Ronda, MBBS, MD2, Enmanuel Then, 3, Pavani Reddy Garlapati, MD1, Jamil Shah, MD1, Vikash Kumar, MD1, Raissa Nana Sede Mbakop, MD4, Hamsika Moparty, MD1, Madhavi Reddy, MD1
1Brooklyn Hospital Center, Brooklyn, NY; 2Mahatma Gandhi Medical College and Research Institute, Pondicherry, India, Brooklyn, NY; 3Universidad Iberoamericana, Gazcue, Distrito Nacional, Dominican Republic; 4Piedmont Athens Regional Medical Center, Athens, GA
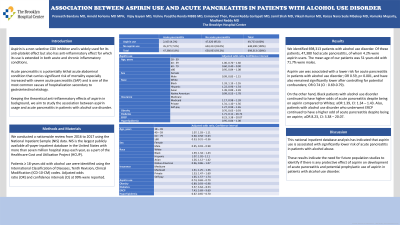
Introduction: Aspirin is a non-selective COX inhibitor and is widely used for its anti-platelet effect but also has anti-inflammatory effect for which its use is extended in both acute and chronic inflammatory conditions. Acute pancreatitis is a potentially lethal acute abdominal condition that carries significant risk of mortality especially increased with severe acute pancreatitis (SAP) and is one of the most common causes of hospitalization secondary to gastrointestinal etiology. Keeping the theoretical anti-inflammatory effects of aspirin in background, we aim to study the association between aspirin usage and acute pancreatitis in patients with alcohol use disorder.
Methods: We conducted a nationwide review from 2016 to 2017 using the National Inpatient Sample (NIS) data. NIS is the largest publicly available all-payer inpatient database in the United States with more than seven million hospital stays each year, as a part of the Healthcare Cost and Utilization Project (HCUP). Patients ≥ 18 years old with alcohol use were identified using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes. Adjusted odds ratio (OR) and confidence intervals (CI) at 99% were reported.
Results: We identified 698,313 patients with alcohol use disorder. Of these patients, 47,380 had acute pancreatitis, of whom 4.2% were aspirin users. The mean age of our patients was 51 years old with 71.7% were males. Aspirin use was associated with a lower risk for acute pancreatitis in patients with alcohol use disorder; OR 0.59, p< 0.001, and have also remained significantly lower after controlling for potential confounders; OR 0.74 (CI : 0.69-0.79).
On the other hand, Black patients with alcohol use disorder continued to have higher odds of acute pancreatitis despite being on aspirin compared to Whites; aOR 1.39, CI: 1.34 – 1.43. Also, patients with alcohol use disorder who underwent ERCP continued to have a higher odd of acute pancreatitis despite being on aspirin; aOR 8.23, CI: 3.38 – 20.07.
Discussion: This national inpatient database analysis has indicated that aspirin use is associated with significantly lower risk of acute pancreatitis in patients with alcohol abuse. These results indicate the need for future population studies to identify if there is any protective effect of aspirin on development of acute pancreatitis and potential prophylactic use of aspirin in patients with alcohol use disorder.
Disclosures:
Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Vijay Gayam, MD1, Vishnu Poojitha Ronda, MBBS, MD2, Enmanuel Then, 3, Pavani Reddy Garlapati, MD1, Jamil Shah, MD1, Vikash Kumar, MD1, Raissa Nana Sede Mbakop, MD4, Hamsika Moparty, MD1, Madhavi Reddy, MD1. P1436 - Association Between Aspirin Use and Acute Pancreatitis in Patients With Alcohol Use Disorder, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2Mahatma Gandhi Medical College and Research Institute, Pondicherry, India, Brooklyn, NY; 3Universidad Iberoamericana, Gazcue, Distrito Nacional, Dominican Republic; 4Piedmont Athens Regional Medical Center, Athens, GA
Introduction: Aspirin is a non-selective COX inhibitor and is widely used for its anti-platelet effect but also has anti-inflammatory effect for which its use is extended in both acute and chronic inflammatory conditions. Acute pancreatitis is a potentially lethal acute abdominal condition that carries significant risk of mortality especially increased with severe acute pancreatitis (SAP) and is one of the most common causes of hospitalization secondary to gastrointestinal etiology. Keeping the theoretical anti-inflammatory effects of aspirin in background, we aim to study the association between aspirin usage and acute pancreatitis in patients with alcohol use disorder.
Methods: We conducted a nationwide review from 2016 to 2017 using the National Inpatient Sample (NIS) data. NIS is the largest publicly available all-payer inpatient database in the United States with more than seven million hospital stays each year, as a part of the Healthcare Cost and Utilization Project (HCUP). Patients ≥ 18 years old with alcohol use were identified using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes. Adjusted odds ratio (OR) and confidence intervals (CI) at 99% were reported.
Results: We identified 698,313 patients with alcohol use disorder. Of these patients, 47,380 had acute pancreatitis, of whom 4.2% were aspirin users. The mean age of our patients was 51 years old with 71.7% were males. Aspirin use was associated with a lower risk for acute pancreatitis in patients with alcohol use disorder; OR 0.59, p< 0.001, and have also remained significantly lower after controlling for potential confounders; OR 0.74 (CI : 0.69-0.79).
On the other hand, Black patients with alcohol use disorder continued to have higher odds of acute pancreatitis despite being on aspirin compared to Whites; aOR 1.39, CI: 1.34 – 1.43. Also, patients with alcohol use disorder who underwent ERCP continued to have a higher odd of acute pancreatitis despite being on aspirin; aOR 8.23, CI: 3.38 – 20.07.
Discussion: This national inpatient database analysis has indicated that aspirin use is associated with significantly lower risk of acute pancreatitis in patients with alcohol abuse. These results indicate the need for future population studies to identify if there is any protective effect of aspirin on development of acute pancreatitis and potential prophylactic use of aspirin in patients with alcohol use disorder.
Disclosures:
Praneeth Bandaru indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Vishnu Poojitha Ronda indicated no relevant financial relationships.
Enmanuel Then indicated no relevant financial relationships.
Pavani Reddy Garlapati indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Raissa Nana Sede Mbakop indicated no relevant financial relationships.
Hamsika Moparty indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Vijay Gayam, MD1, Vishnu Poojitha Ronda, MBBS, MD2, Enmanuel Then, 3, Pavani Reddy Garlapati, MD1, Jamil Shah, MD1, Vikash Kumar, MD1, Raissa Nana Sede Mbakop, MD4, Hamsika Moparty, MD1, Madhavi Reddy, MD1. P1436 - Association Between Aspirin Use and Acute Pancreatitis in Patients With Alcohol Use Disorder, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
