Monday Poster Session
Category: Biliary/Pancreas
P1440 - Development of a Model to Predict Post-Acute Pancreatitis Diabetes
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Harry Trieu, MD
Keck School of Medicine of USC
Los Angeles, CA
Presenting Author(s)
Award: Presidential Poster Award
Harry Trieu, MD1, Aneesa Chowdhury, MD1, Jennifer L. Dodge, MPH2, Stephen Pandol, MD3, Marc Goodarzi, MD, PhD3, Ira Shulman, MD1, Christie Jeon, PhD3, James Buxbaum, MD, MS1
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Acute pancreatitis (AP) is the most common gastrointestinal cause for hospital admission in the United States. A significant proportion of patients will develop post-pancreatitis diabetes mellitus (PPDM-A) several years of their index admission. We aimed to develop a predictive model to help clinicians identify patients at risk for developing PPDM-A.
Methods: A prospective cohort of patients aged 18 or older presenting to LAC+USC Medical Center with a diagnosis of acute pancreatitis according to the Revised Atlanta Criteria between March 2015 and March 2022 was used to build the model. Patients with a diagnosis of diabetes that preceded their index admission for AP were excluded. Patients with a hemoglobin A1c>6.5% or documentation of a diabetes diagnosis after index admission for AP were deemed to have developed PPDM-A.
The dataset was then divided into training and testing sets with 75% and 25% of patients assigned to each, respectively. An elastic net regression model was fit on the training set to select variables correlated with the development of PPDM-A. We then validated the model on previously unseen data (the testing set) and calculated an area under the receiver operator characteristic curve (AUROC).
Results: One thousand and twenty-three patients with median age 42 years, 80.4% Hispanic, and 45.9% female met inclusion criteria for this study (Table). The most common AP etiology was gallstones, seen in 488 (47.7%) patients, followed by alcohol, seen in 275 (26.9%) patients. The training and testing sets consisted of 767 and 256 patients. Thirty-six patients (3.5%) developed PPDM-A.
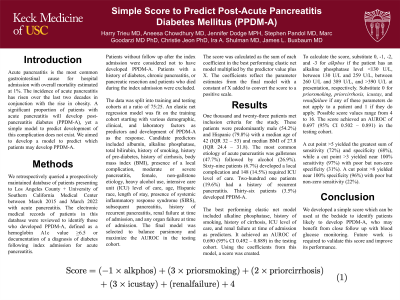
The best performing elastic net model included alkaline phosphatase, history of smoking, history of pre-diabetes, history of cirrhosis, moderate or severe pancreatitis, ICU level of care, and history of recurrent pancreatitis as predictors (Figure 1). It achieved an AUROC of 0.78 (95% CI 0.69-0.86) in the training and 0.81 (95% CI 0.64-0.98) in the testing set.
Discussion: In this study, we developed an elastic net regression model which predicts development of PPDM-A and achieves an AUROC of 0.81 (95% CI 0.64-0.98) in unseen data. Pending external validation, this model may help clinicians identify patients at risk for developing this serious complication and guide early treatment.

Disclosures:
Harry Trieu, MD1, Aneesa Chowdhury, MD1, Jennifer L. Dodge, MPH2, Stephen Pandol, MD3, Marc Goodarzi, MD, PhD3, Ira Shulman, MD1, Christie Jeon, PhD3, James Buxbaum, MD, MS1. P1440 - Development of a Model to Predict Post-Acute Pancreatitis Diabetes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Harry Trieu, MD1, Aneesa Chowdhury, MD1, Jennifer L. Dodge, MPH2, Stephen Pandol, MD3, Marc Goodarzi, MD, PhD3, Ira Shulman, MD1, Christie Jeon, PhD3, James Buxbaum, MD, MS1
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Acute pancreatitis (AP) is the most common gastrointestinal cause for hospital admission in the United States. A significant proportion of patients will develop post-pancreatitis diabetes mellitus (PPDM-A) several years of their index admission. We aimed to develop a predictive model to help clinicians identify patients at risk for developing PPDM-A.
Methods: A prospective cohort of patients aged 18 or older presenting to LAC+USC Medical Center with a diagnosis of acute pancreatitis according to the Revised Atlanta Criteria between March 2015 and March 2022 was used to build the model. Patients with a diagnosis of diabetes that preceded their index admission for AP were excluded. Patients with a hemoglobin A1c>6.5% or documentation of a diabetes diagnosis after index admission for AP were deemed to have developed PPDM-A.
The dataset was then divided into training and testing sets with 75% and 25% of patients assigned to each, respectively. An elastic net regression model was fit on the training set to select variables correlated with the development of PPDM-A. We then validated the model on previously unseen data (the testing set) and calculated an area under the receiver operator characteristic curve (AUROC).
Results: One thousand and twenty-three patients with median age 42 years, 80.4% Hispanic, and 45.9% female met inclusion criteria for this study (Table). The most common AP etiology was gallstones, seen in 488 (47.7%) patients, followed by alcohol, seen in 275 (26.9%) patients. The training and testing sets consisted of 767 and 256 patients. Thirty-six patients (3.5%) developed PPDM-A.
The best performing elastic net model included alkaline phosphatase, history of smoking, history of pre-diabetes, history of cirrhosis, moderate or severe pancreatitis, ICU level of care, and history of recurrent pancreatitis as predictors (Figure 1). It achieved an AUROC of 0.78 (95% CI 0.69-0.86) in the training and 0.81 (95% CI 0.64-0.98) in the testing set.
Discussion: In this study, we developed an elastic net regression model which predicts development of PPDM-A and achieves an AUROC of 0.81 (95% CI 0.64-0.98) in unseen data. Pending external validation, this model may help clinicians identify patients at risk for developing this serious complication and guide early treatment.

Figure: Prediction model of diabetes after acute pancreatitis
Disclosures:
Harry Trieu indicated no relevant financial relationships.
Aneesa Chowdhury indicated no relevant financial relationships.
Jennifer Dodge indicated no relevant financial relationships.
Stephen Pandol indicated no relevant financial relationships.
Marc Goodarzi indicated no relevant financial relationships.
Ira Shulman indicated no relevant financial relationships.
Christie Jeon indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Harry Trieu, MD1, Aneesa Chowdhury, MD1, Jennifer L. Dodge, MPH2, Stephen Pandol, MD3, Marc Goodarzi, MD, PhD3, Ira Shulman, MD1, Christie Jeon, PhD3, James Buxbaum, MD, MS1. P1440 - Development of a Model to Predict Post-Acute Pancreatitis Diabetes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

