Monday Poster Session
Category: Biliary/Pancreas
P1449 - Outcomes of Acute Pancreatitis Hospitalization in Patients With Inflammatory Bowel Disease: A Nationwide Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
- FJ
Fangyuan Jin-Dominguez, MD
Case Western Reserve / University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Fangyuan Jin-Dominguez, MD1, Abbinaya Elangovan, MD2, Khadija Naseem, MD3, Ahmad Khan, MD2, Emad Mansoor, MD4, Gregory Cooper, MD2, Jeffry Katz, MD2, Vu Nguyen, MD2
1Case Western Reserve / University Hospitals Cleveland Medical Center, Cleveland, OH; 2Case Western Reserve/UHCMC, Cleveland, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Case Western Reserve University / University Hospitals, Cleveland, OH
Introduction: Prior studies have demonstrated an increased risk of pancreatitis in patients with inflammatory bowel disease (IBD). However, there are limited data on outcomes of acute pancreatitis (AP) hospitalization in IBD patients. Using the nationwide inpatient sample (NIS), we evaluated patient characteristics, etiology and severity of AP in hospitalized IBD patients.
Methods: The NIS was queried from January 1st, 2016 to December 31st, 2020, utilizing ICD-10 diagnosis codes to identify patients hospitalized with AP with and without IBD. We excluded patients younger than 18 years. We collected data on patient demographics, comorbidities, etiology, severity of AP including mortality, length of stay (LOS), and cost of hospitalization. We performed chi-square test for categorical data and student t-test for continuous data to test statistical significance.
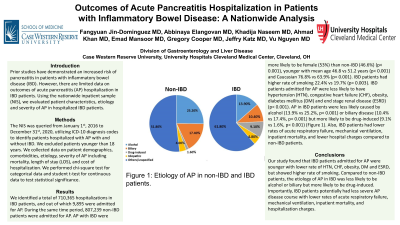
Results: We identified a total of 710,365 hospitalizations in IBD patients, and out of which 9,895 were admitted for AP. During the same time period, 807,239 non-IBD patients were admitted for AP. AP with IBD were more likely to be female (53%) than non-IBD (46.6%) (p< 0.001), younger with mean age 46.8 vs 51.2 years (p< 0.001) and Caucasian 76.8% vs 63.9% (p< 0.001) (Table 1). IBD patients had higher rate of smoking 22.4% vs 19.7% (p= 0.003) (Table 1). IBD patients admitted for AP were less likely to have hypertension (HTN), congestive heart failure (CHF), obesity, diabetes mellitus (DM) and end stage renal disease (ESRD) (p< 0.001) (Table 1). AP in IBD patients were less likely caused by alcohol (13.9% vs 25.2%, p< 0.001) or biliary disease (10.4% vs 17.4%, p< 0.001) but more likely to be drug-induced (9.1% vs 1.6%, p< 0.001) (Figure 1). Also, IBD patients had lower rates of acute respiratory failure, mechanical ventilation, inpatient mortality, and lower hospital charges compared to non-IBD patients (Table 1).
Discussion: Our study found that IBD patients admitted for AP were younger with lower rate of HTN, CHF, obesity, DM and ESRD, but showed higher rate of smoking. Compared to non-IBD patients, the etiology of AP in IBD was less likely to be alcohol or biliary but more likely to be drug-induced. Importantly, IBD patients potentially had less severe AP disease course with lower rates of acute respiratory failure, mechanical ventilation, inpatient mortality, and hospitalization charges.

Disclosures:
Fangyuan Jin-Dominguez, MD1, Abbinaya Elangovan, MD2, Khadija Naseem, MD3, Ahmad Khan, MD2, Emad Mansoor, MD4, Gregory Cooper, MD2, Jeffry Katz, MD2, Vu Nguyen, MD2. P1449 - Outcomes of Acute Pancreatitis Hospitalization in Patients With Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve / University Hospitals Cleveland Medical Center, Cleveland, OH; 2Case Western Reserve/UHCMC, Cleveland, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Case Western Reserve University / University Hospitals, Cleveland, OH
Introduction: Prior studies have demonstrated an increased risk of pancreatitis in patients with inflammatory bowel disease (IBD). However, there are limited data on outcomes of acute pancreatitis (AP) hospitalization in IBD patients. Using the nationwide inpatient sample (NIS), we evaluated patient characteristics, etiology and severity of AP in hospitalized IBD patients.
Methods: The NIS was queried from January 1st, 2016 to December 31st, 2020, utilizing ICD-10 diagnosis codes to identify patients hospitalized with AP with and without IBD. We excluded patients younger than 18 years. We collected data on patient demographics, comorbidities, etiology, severity of AP including mortality, length of stay (LOS), and cost of hospitalization. We performed chi-square test for categorical data and student t-test for continuous data to test statistical significance.
Results: We identified a total of 710,365 hospitalizations in IBD patients, and out of which 9,895 were admitted for AP. During the same time period, 807,239 non-IBD patients were admitted for AP. AP with IBD were more likely to be female (53%) than non-IBD (46.6%) (p< 0.001), younger with mean age 46.8 vs 51.2 years (p< 0.001) and Caucasian 76.8% vs 63.9% (p< 0.001) (Table 1). IBD patients had higher rate of smoking 22.4% vs 19.7% (p= 0.003) (Table 1). IBD patients admitted for AP were less likely to have hypertension (HTN), congestive heart failure (CHF), obesity, diabetes mellitus (DM) and end stage renal disease (ESRD) (p< 0.001) (Table 1). AP in IBD patients were less likely caused by alcohol (13.9% vs 25.2%, p< 0.001) or biliary disease (10.4% vs 17.4%, p< 0.001) but more likely to be drug-induced (9.1% vs 1.6%, p< 0.001) (Figure 1). Also, IBD patients had lower rates of acute respiratory failure, mechanical ventilation, inpatient mortality, and lower hospital charges compared to non-IBD patients (Table 1).
Discussion: Our study found that IBD patients admitted for AP were younger with lower rate of HTN, CHF, obesity, DM and ESRD, but showed higher rate of smoking. Compared to non-IBD patients, the etiology of AP in IBD was less likely to be alcohol or biliary but more likely to be drug-induced. Importantly, IBD patients potentially had less severe AP disease course with lower rates of acute respiratory failure, mechanical ventilation, inpatient mortality, and hospitalization charges.

Figure: Figure 1: Etiology of AP in non-IBD and IBD patients.
Disclosures:
Fangyuan Jin-Dominguez indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Khadija Naseem indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Jeffry Katz: Janssen, Pharmaceuticals – Grant/Research Support.
Vu Nguyen: AbbVie – Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member.
Fangyuan Jin-Dominguez, MD1, Abbinaya Elangovan, MD2, Khadija Naseem, MD3, Ahmad Khan, MD2, Emad Mansoor, MD4, Gregory Cooper, MD2, Jeffry Katz, MD2, Vu Nguyen, MD2. P1449 - Outcomes of Acute Pancreatitis Hospitalization in Patients With Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
