Monday Poster Session
Category: Biliary/Pancreas
P1460 - Destination Therapy Reduces the Incidence of Disconnected Pancreatic Duct Syndrome in Walled Off Necrosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- WW
William H. Wheless, MD
Atrium Health Carolinas Medical Center
Charlotte, NC
Presenting Author(s)
William H. Wheless, MD1, Robert A. Moran, MD2
1Atrium Health Carolinas Medical Center, Charlotte, NC; 2Medical University of South Carolina, Charleston, SC
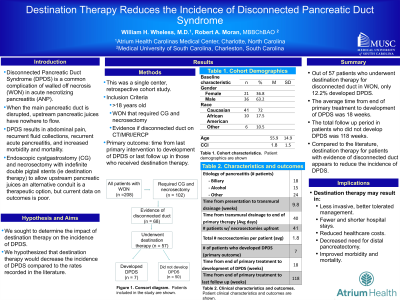
Introduction: Disconnected pancreatic duct syndrome (DPDS) is a complication of Acute Necrotizing Pancreatitis (ANP) that occurs due to walled off necrosis (WON) causing disruption of the main pancreatic duct. DPDS results in significant abdominal pain, recurrent fluid collections, recurrent acute pancreatitis, and overall increased morbidity and mortality. DPDS is observed in up to 50% of patients with ANP (1). One therapeutic option is endoscopic cystgastrostomy with transmural drainage with indefinite double pigtail stents (ie destination therapy) to allow upstream pancreatic juices an alternative conduit. Current data on the outcomes of this procedure is limited. The aim of this study is to evaluate the impact of destination therapy on the incidence of DPDS.
Methods: This is a single center, retrospective study. Patients who underwent transmural drainage of walled off pancreatic necrosis were identified using the electronic medical record from February 2014 to July 2022. Inclusion criteria were those age > 18 who had evidence of WON and disrupted duct on imaging (CT or MRCP) or ERCP. Primary outcome was time from last primary intervention to development of DPDS or last follow up in those who received destination therapy.
Results: A total of 284 patients had evidence of WON on imaging. 102 (35.9%) of these patients required endoscopic CG. Of those who required CG, 68 (66.7%) had evidence of disconnected duct. Of the patients who had disconneted ducts, 57 (83.8%) of these patients underwent destination therapy. Of those who underwent destination therapy, 8 (14.0%) developed disconnected pancreatic duct syndrome. Of those who did not develop DPDS, average follow up was 103.11 weeks. The average number of necrosectomies performed per patient was 1.8.
Discussion: Our data suggests that destination therapy for patients with WON who have evidence of disconnected pancreatic duct on imaging may prevent DPDS. Implications include less invasive management, decreased hospitalizations, overall decreased healthcare costs as well as overall improved morbidity and mortality. Further studies are warranted to determine the optimal method to prevent DPDS.
References
1. Varadarajulu S. Wilcox C.M. Endoscopic placement of permanent indwelling transmural stents in disconnected pancreatic duct syndrome: does benefit outweigh the risks?. Gastrointest Endosc. 2011; 74: 1408-1412
Disclosures:
William H. Wheless, MD1, Robert A. Moran, MD2. P1460 - Destination Therapy Reduces the Incidence of Disconnected Pancreatic Duct Syndrome in Walled Off Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Atrium Health Carolinas Medical Center, Charlotte, NC; 2Medical University of South Carolina, Charleston, SC
Introduction: Disconnected pancreatic duct syndrome (DPDS) is a complication of Acute Necrotizing Pancreatitis (ANP) that occurs due to walled off necrosis (WON) causing disruption of the main pancreatic duct. DPDS results in significant abdominal pain, recurrent fluid collections, recurrent acute pancreatitis, and overall increased morbidity and mortality. DPDS is observed in up to 50% of patients with ANP (1). One therapeutic option is endoscopic cystgastrostomy with transmural drainage with indefinite double pigtail stents (ie destination therapy) to allow upstream pancreatic juices an alternative conduit. Current data on the outcomes of this procedure is limited. The aim of this study is to evaluate the impact of destination therapy on the incidence of DPDS.
Methods: This is a single center, retrospective study. Patients who underwent transmural drainage of walled off pancreatic necrosis were identified using the electronic medical record from February 2014 to July 2022. Inclusion criteria were those age > 18 who had evidence of WON and disrupted duct on imaging (CT or MRCP) or ERCP. Primary outcome was time from last primary intervention to development of DPDS or last follow up in those who received destination therapy.
Results: A total of 284 patients had evidence of WON on imaging. 102 (35.9%) of these patients required endoscopic CG. Of those who required CG, 68 (66.7%) had evidence of disconnected duct. Of the patients who had disconneted ducts, 57 (83.8%) of these patients underwent destination therapy. Of those who underwent destination therapy, 8 (14.0%) developed disconnected pancreatic duct syndrome. Of those who did not develop DPDS, average follow up was 103.11 weeks. The average number of necrosectomies performed per patient was 1.8.
Discussion: Our data suggests that destination therapy for patients with WON who have evidence of disconnected pancreatic duct on imaging may prevent DPDS. Implications include less invasive management, decreased hospitalizations, overall decreased healthcare costs as well as overall improved morbidity and mortality. Further studies are warranted to determine the optimal method to prevent DPDS.
References
1. Varadarajulu S. Wilcox C.M. Endoscopic placement of permanent indwelling transmural stents in disconnected pancreatic duct syndrome: does benefit outweigh the risks?. Gastrointest Endosc. 2011; 74: 1408-1412
Disclosures:
William Wheless indicated no relevant financial relationships.
Robert Moran indicated no relevant financial relationships.
William H. Wheless, MD1, Robert A. Moran, MD2. P1460 - Destination Therapy Reduces the Incidence of Disconnected Pancreatic Duct Syndrome in Walled Off Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
