Monday Poster Session
Category: Biliary/Pancreas
P1461 - ERCP Intervention for Biliary Strictures: The Comparison Between Living and Deceased Donor Liver Transplants
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Sara Kiparizoska, MD
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Sara Kiparizoska, MD1, Stephanie M. Woo, MD1, Ade Waterman, MBChB1, Obada Tabbaa, MD1, Mai Dabbas, BA2, Joseph Clinton, MD3, Walid Chalhoub, MD1, Mark Real, MD1, Nadim Haddad, MD1
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University School of Medicine, Washington, DC; 3University of Maryland Medical Center, Baltimore, MD
Introduction: Biliary complications account for 10-25% of all complications after liver transplant and are more commonly seen in live donor liver transplants (LDLT) compared to deceased donor liver transplants (DDLT). The objective of this study was to compare outcomes between DDLT and LDLT who underwent endoscopic retrograde cholangiopancreatography (ERCP) treatment to resolve post-transplant biliary complications.
Methods: We conducted a retrospective chart review of patients who had ERCP following liver transplant from September 2011 to January 2022. Outcomes included treatment failure, defined as the need for surgery or interventional radiology (IR) referral, and graft failure, defined as the need for a repeat transplant. Chi-square tests and t- tests were used for analysis.
Results: In total, 5 of the 77 patients received a LDLT (6.5%) and the remaining received DDLT. Stents were placed in 60% of the LDLT (3/5) and 88% of the DDLT (63/72). Treatment failure occurred in 40% of LDLT and 8.3% of the DDLT (p= 0.025). Graft failure was not observed in LDLT and 2.8% of the DDLT. Of patients who received DDLT, 87.5% were deceased after brain death (DBD) (63/72) and 12.5% were deceased after cardiac death (DCD) (9/72). Treatment failure was observed in 7.9% of DBD grafts vs. 11.1% of DCD grafts (p=0.747). One DBD graft and one DCD graft had graft failure, needing a repeat transplant (p=0.008). For patients who had a follow up ERCP, 80% of DDLT (47/59) and 25% of LDLT (1/4) had persistent strictures (p=0.019).
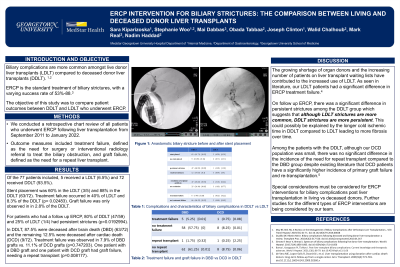
Discussion: The shortage of organ donors and the increasing number of patients on liver transplant lists have contributed to the increased use of LDLT. Anastomotic biliary strictures as seen in Figure 1 most often appear in LDLT and less often in DDLT. Our LDLT patients had a significant difference in treatment failure which led to more referrals to surgery and IR to treat the biliary obstruction.
On initial follow up ERCP, there was a significant difference in persistent strictures among the DDLT. Although our study has a small LDLT donor sample size at a single center, it suggests that although LDLT strictures are more common, DDLT strictures are more persistent. This could possibly be explained by the longer cold ischemic time in DDLT compared to LDLT leading to more fibrosis. Special considerations must be considered for ERCP interventions for biliary complications post liver transplantation in living vs deceased donors and different types of ERCP interventions are being considered by our team.

Disclosures:
Sara Kiparizoska, MD1, Stephanie M. Woo, MD1, Ade Waterman, MBChB1, Obada Tabbaa, MD1, Mai Dabbas, BA2, Joseph Clinton, MD3, Walid Chalhoub, MD1, Mark Real, MD1, Nadim Haddad, MD1. P1461 - ERCP Intervention for Biliary Strictures: The Comparison Between Living and Deceased Donor Liver Transplants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University School of Medicine, Washington, DC; 3University of Maryland Medical Center, Baltimore, MD
Introduction: Biliary complications account for 10-25% of all complications after liver transplant and are more commonly seen in live donor liver transplants (LDLT) compared to deceased donor liver transplants (DDLT). The objective of this study was to compare outcomes between DDLT and LDLT who underwent endoscopic retrograde cholangiopancreatography (ERCP) treatment to resolve post-transplant biliary complications.
Methods: We conducted a retrospective chart review of patients who had ERCP following liver transplant from September 2011 to January 2022. Outcomes included treatment failure, defined as the need for surgery or interventional radiology (IR) referral, and graft failure, defined as the need for a repeat transplant. Chi-square tests and t- tests were used for analysis.
Results: In total, 5 of the 77 patients received a LDLT (6.5%) and the remaining received DDLT. Stents were placed in 60% of the LDLT (3/5) and 88% of the DDLT (63/72). Treatment failure occurred in 40% of LDLT and 8.3% of the DDLT (p= 0.025). Graft failure was not observed in LDLT and 2.8% of the DDLT. Of patients who received DDLT, 87.5% were deceased after brain death (DBD) (63/72) and 12.5% were deceased after cardiac death (DCD) (9/72). Treatment failure was observed in 7.9% of DBD grafts vs. 11.1% of DCD grafts (p=0.747). One DBD graft and one DCD graft had graft failure, needing a repeat transplant (p=0.008). For patients who had a follow up ERCP, 80% of DDLT (47/59) and 25% of LDLT (1/4) had persistent strictures (p=0.019).
Discussion: The shortage of organ donors and the increasing number of patients on liver transplant lists have contributed to the increased use of LDLT. Anastomotic biliary strictures as seen in Figure 1 most often appear in LDLT and less often in DDLT. Our LDLT patients had a significant difference in treatment failure which led to more referrals to surgery and IR to treat the biliary obstruction.
On initial follow up ERCP, there was a significant difference in persistent strictures among the DDLT. Although our study has a small LDLT donor sample size at a single center, it suggests that although LDLT strictures are more common, DDLT strictures are more persistent. This could possibly be explained by the longer cold ischemic time in DDLT compared to LDLT leading to more fibrosis. Special considerations must be considered for ERCP interventions for biliary complications post liver transplantation in living vs deceased donors and different types of ERCP interventions are being considered by our team.

Figure: Figure 1: Anastomotic biliary stricture before and after stent placement
Disclosures:
Sara Kiparizoska indicated no relevant financial relationships.
Stephanie Woo indicated no relevant financial relationships.
Ade Waterman indicated no relevant financial relationships.
Obada Tabbaa indicated no relevant financial relationships.
Mai Dabbas indicated no relevant financial relationships.
Joseph Clinton indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Mark Real indicated no relevant financial relationships.
Nadim Haddad indicated no relevant financial relationships.
Sara Kiparizoska, MD1, Stephanie M. Woo, MD1, Ade Waterman, MBChB1, Obada Tabbaa, MD1, Mai Dabbas, BA2, Joseph Clinton, MD3, Walid Chalhoub, MD1, Mark Real, MD1, Nadim Haddad, MD1. P1461 - ERCP Intervention for Biliary Strictures: The Comparison Between Living and Deceased Donor Liver Transplants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
