Monday Poster Session
Category: Biliary/Pancreas
P1476 - A Rare Case of Sigmoid Colon Perforation in Severe Acute Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HS
Hasan Saleh, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Hasan Saleh, MD1, Induja R. Nimma, MD1, Yuting Huang, MBBS, PhD2, Dana Amiraian, MD1, Maoyin Pang, MD, PhD2, Michelle DeLeon, MD1, Michele Lewis, MD1, Jana G.. Hashash, MD, MSc, FACG1
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL
Introduction: Severe acute pancreatitis (AP) can cause systemic complications and can lead to organ failure including renal failure, respiratory failure, among others increasing the risk of associated morbidity and mortality. Balthazar score grades AP severity based on CT imaging and extent of necrosis. Bowel complications associated with AP are rare. Extravasation of pancreatic enzymes into the abdominal cavity can cause an inflammatory reaction leading to bowel wall inflammation and possible progression to bowel ischemia, necrosis, or perforation.
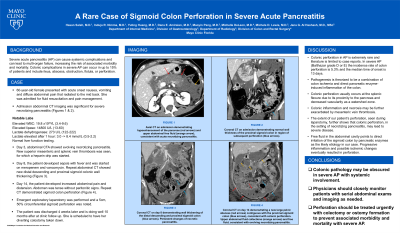
Case Description/Methods: A 60-year-old female with history of eosinophilic esophagitis presented with acute onset nausea, vomiting and diffuse abdominal pain that radiated to the mid back. Initial abdominal exam revealed generalized tenderness without rigidity. Labs showed lipase 14,800 U/L (13-60), WBC 19.8 x10(9)/L (3.4-9.6), AST 30 U/L (8-43), ALT 22 U/L (7-45), ALP 90 U/L (35-104), T Bil 0.5 mg/dL (< 1.2), D Bil 0.1 mg/dL (< 0.3), and lactate 3.0 mmol/L (0.5-2.2). Abdominopelvic CT with contrast showed severe necrotizing pancreatitis with abdominopelvic free fluid. She was admitted for fluid resuscitation and pain management. Hospital course was complicated by SMV thrombosis and ARDS. Fourteen days into admission, the patient had acute worsening abdominal pain with new fever and leukocytosis meeting 2/4 SIRS criteria. Physical exam revealed a distended, tender, and tense abdomen. Repeat CT with contrast showed a new large collection of fluid and gas contiguous with the proximal sigmoid colon and small free air. Emergent exploratory laparotomy revealed pancreatic fluid in the abdomen with 5 cm perforation of the sigmoid colon anterior wall. Transverse loop colostomy was performed with placement of two abdominal drains . She was discharged home 4 weeks later.
Discussion: Colonic perforation in patients with AP is extremely uncommon, with literature limited to case reports. In patients with severe AP (Balthazar grade D or E), the incidence of colon perforation is 5.3% and the median time of onset is 13 days.1 Colonic pathology may be obscured in severe AP with systemic involvement.2 Physicians should closely monitor with serial abdominal exams and imaging as needed.
1. Nakanishi N et al. CT evaluation and clinical factors predicting delayed colonic perforation following acute pancreatitis. 2016. 10-15.
2. Nagpal A et al. Severe Colonic Complications requiring Sub-Total Colectomy in Acute Necrotizing Pancreatitis—A Retrospective Study of 8 patients. 2012.

Disclosures:
Hasan Saleh, MD1, Induja R. Nimma, MD1, Yuting Huang, MBBS, PhD2, Dana Amiraian, MD1, Maoyin Pang, MD, PhD2, Michelle DeLeon, MD1, Michele Lewis, MD1, Jana G.. Hashash, MD, MSc, FACG1. P1476 - A Rare Case of Sigmoid Colon Perforation in Severe Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL
Introduction: Severe acute pancreatitis (AP) can cause systemic complications and can lead to organ failure including renal failure, respiratory failure, among others increasing the risk of associated morbidity and mortality. Balthazar score grades AP severity based on CT imaging and extent of necrosis. Bowel complications associated with AP are rare. Extravasation of pancreatic enzymes into the abdominal cavity can cause an inflammatory reaction leading to bowel wall inflammation and possible progression to bowel ischemia, necrosis, or perforation.
Case Description/Methods: A 60-year-old female with history of eosinophilic esophagitis presented with acute onset nausea, vomiting and diffuse abdominal pain that radiated to the mid back. Initial abdominal exam revealed generalized tenderness without rigidity. Labs showed lipase 14,800 U/L (13-60), WBC 19.8 x10(9)/L (3.4-9.6), AST 30 U/L (8-43), ALT 22 U/L (7-45), ALP 90 U/L (35-104), T Bil 0.5 mg/dL (< 1.2), D Bil 0.1 mg/dL (< 0.3), and lactate 3.0 mmol/L (0.5-2.2). Abdominopelvic CT with contrast showed severe necrotizing pancreatitis with abdominopelvic free fluid. She was admitted for fluid resuscitation and pain management. Hospital course was complicated by SMV thrombosis and ARDS. Fourteen days into admission, the patient had acute worsening abdominal pain with new fever and leukocytosis meeting 2/4 SIRS criteria. Physical exam revealed a distended, tender, and tense abdomen. Repeat CT with contrast showed a new large collection of fluid and gas contiguous with the proximal sigmoid colon and small free air. Emergent exploratory laparotomy revealed pancreatic fluid in the abdomen with 5 cm perforation of the sigmoid colon anterior wall. Transverse loop colostomy was performed with placement of two abdominal drains . She was discharged home 4 weeks later.
Discussion: Colonic perforation in patients with AP is extremely uncommon, with literature limited to case reports. In patients with severe AP (Balthazar grade D or E), the incidence of colon perforation is 5.3% and the median time of onset is 13 days.1 Colonic pathology may be obscured in severe AP with systemic involvement.2 Physicians should closely monitor with serial abdominal exams and imaging as needed.
1. Nakanishi N et al. CT evaluation and clinical factors predicting delayed colonic perforation following acute pancreatitis. 2016. 10-15.
2. Nagpal A et al. Severe Colonic Complications requiring Sub-Total Colectomy in Acute Necrotizing Pancreatitis—A Retrospective Study of 8 patients. 2012.

Figure: Coronal CT image demonstrating large abscess (red arrows) contiguous with the proximal sigmoid colon (blue arrows), consistent with colonic perforation. Upper abdominal fluid collections (orange arrows) and free fluid, consistent with necrotizing pancreatitis.
Disclosures:
Hasan Saleh indicated no relevant financial relationships.
Induja Nimma indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Dana Amiraian indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
Michelle DeLeon indicated no relevant financial relationships.
Michele Lewis indicated no relevant financial relationships.
Jana Hashash: Iterative Health – Grant/Research Support.
Hasan Saleh, MD1, Induja R. Nimma, MD1, Yuting Huang, MBBS, PhD2, Dana Amiraian, MD1, Maoyin Pang, MD, PhD2, Michelle DeLeon, MD1, Michele Lewis, MD1, Jana G.. Hashash, MD, MSc, FACG1. P1476 - A Rare Case of Sigmoid Colon Perforation in Severe Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
