Monday Poster Session
Category: Biliary/Pancreas
P1480 - A Delayed Diagnosis of Autoimmune Pancreatitis in a Patient With Alcohol Use Disorder
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Andre Khazak, DO
Mount Sinai Beth Israel
New York, New York
Presenting Author(s)
Andre Khazak, DO1, Patricia Miguez Arosemena, MD2, Jake Debroff, MD1, Violetta Laskova, MD1
1Mount Sinai Beth Israel, New York, NY; 2Mount Sinai West and Morningside, New York, NY
Introduction: Autoimmune pancreatitis (AIP) is a rare etiology of pancreatic inflammation that can have presentations ranging from asymptomatic jaundice to severe abdominal pain. Type 2 AIP has a younger age of onset, often without significant elevation in immunoglobulin G4 (IgG4) positive cells and a lack of systemic involvement as compared to type 1 AIP. Diagnosis is based on imaging, histology, and IgG4 levels with consideration for response to glucocorticoids. We present a case of a 28-year-old male with 7 emergency department (ED) visits for abdominal pain thought to be secondary to alcohol related pancreatitis found to have repeat imaging concerning for AIP.
Case Description/Methods: A 28-year old male with a history of alcohol use disorder presented to the ED for recurrent abdominal pain, his 7th ED visit over a 2-week interval. He had elevated lipase levels ranging from 609 U/L to 1,141 U/L on previous visits treated with fluids and nonsteroidal anti-inflammatory drugs without further work up given presumptive diagnosis of alcohol related pancreatitis. Initial CT scan obtained during his 5th ED visit showed haziness in the pancreatic head and body consistent with acute pancreatitis without necrosis. Ultrasound was negative for gallstones. The patient was again discharged following pain control. During his 7th and final ED visit, the patient endorsed additional symptoms of dark urine and clay colored stool. Labs were significant for an elevated lipase to 344 U/L with new transaminitis with AST 339 U/L, ALT 699 U/L, direct bilirubin 5.6 mg/dl, and total bilirubin 7.4 mg/dl. Repeat CT revealed acute pancreatitis with new hyperenhancement of the pancreatic tail with intra and extra hepatic bile duct dilatation with abrupt tapering of the common bile duct (CBD). MRCP revealed a diffusely boggy, enlarged sausage-shaped pancreas and distal CBD narrowing with upstream CBD dilatation suspicious for autoimmune pancreatitis. IgG4 levels returned elevated to 101 mg/dl after the patient had left against medical advice and subsequently lost to follow up.
Discussion: AIP is a rare and often missed diagnosis. Lack of suspicion for AIP in this patient with alcohol use disorder resulted in delayed diagnosis and failure to administer steroids leading to recurrent ED visits. Physicians need to be diligent in considering an immunologic component of pancreatitis in young patients as early diagnosis will provide prompt initiation of appropriate serologic and radiologic work up with timely initiation of steroids.

Disclosures:
Andre Khazak, DO1, Patricia Miguez Arosemena, MD2, Jake Debroff, MD1, Violetta Laskova, MD1. P1480 - A Delayed Diagnosis of Autoimmune Pancreatitis in a Patient With Alcohol Use Disorder, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Beth Israel, New York, NY; 2Mount Sinai West and Morningside, New York, NY
Introduction: Autoimmune pancreatitis (AIP) is a rare etiology of pancreatic inflammation that can have presentations ranging from asymptomatic jaundice to severe abdominal pain. Type 2 AIP has a younger age of onset, often without significant elevation in immunoglobulin G4 (IgG4) positive cells and a lack of systemic involvement as compared to type 1 AIP. Diagnosis is based on imaging, histology, and IgG4 levels with consideration for response to glucocorticoids. We present a case of a 28-year-old male with 7 emergency department (ED) visits for abdominal pain thought to be secondary to alcohol related pancreatitis found to have repeat imaging concerning for AIP.
Case Description/Methods: A 28-year old male with a history of alcohol use disorder presented to the ED for recurrent abdominal pain, his 7th ED visit over a 2-week interval. He had elevated lipase levels ranging from 609 U/L to 1,141 U/L on previous visits treated with fluids and nonsteroidal anti-inflammatory drugs without further work up given presumptive diagnosis of alcohol related pancreatitis. Initial CT scan obtained during his 5th ED visit showed haziness in the pancreatic head and body consistent with acute pancreatitis without necrosis. Ultrasound was negative for gallstones. The patient was again discharged following pain control. During his 7th and final ED visit, the patient endorsed additional symptoms of dark urine and clay colored stool. Labs were significant for an elevated lipase to 344 U/L with new transaminitis with AST 339 U/L, ALT 699 U/L, direct bilirubin 5.6 mg/dl, and total bilirubin 7.4 mg/dl. Repeat CT revealed acute pancreatitis with new hyperenhancement of the pancreatic tail with intra and extra hepatic bile duct dilatation with abrupt tapering of the common bile duct (CBD). MRCP revealed a diffusely boggy, enlarged sausage-shaped pancreas and distal CBD narrowing with upstream CBD dilatation suspicious for autoimmune pancreatitis. IgG4 levels returned elevated to 101 mg/dl after the patient had left against medical advice and subsequently lost to follow up.
Discussion: AIP is a rare and often missed diagnosis. Lack of suspicion for AIP in this patient with alcohol use disorder resulted in delayed diagnosis and failure to administer steroids leading to recurrent ED visits. Physicians need to be diligent in considering an immunologic component of pancreatitis in young patients as early diagnosis will provide prompt initiation of appropriate serologic and radiologic work up with timely initiation of steroids.

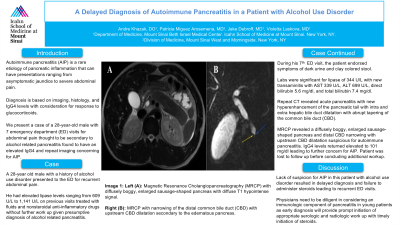
Figure: Left (A): Magnetic Resonance Cholangiopancreatography (MRCP) with diffusely boggy, enlarged sausage-shaped pancreas with diffuse T1 hypointense signal.
Right (B): MRCP with narrowing of the distal common bile duct (CBD) with upstream CBD dilatation secondary to the edematous pancreas.
Right (B): MRCP with narrowing of the distal common bile duct (CBD) with upstream CBD dilatation secondary to the edematous pancreas.
Disclosures:
Andre Khazak indicated no relevant financial relationships.
Patricia Miguez Arosemena indicated no relevant financial relationships.
Jake Debroff indicated no relevant financial relationships.
Violetta Laskova indicated no relevant financial relationships.
Andre Khazak, DO1, Patricia Miguez Arosemena, MD2, Jake Debroff, MD1, Violetta Laskova, MD1. P1480 - A Delayed Diagnosis of Autoimmune Pancreatitis in a Patient With Alcohol Use Disorder, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
