Monday Poster Session
Category: Biliary/Pancreas
P1483 - Stent Gone Rogue - Long Standing Cystgastrostomy Stent Eroding into the Common Bile Duct
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Amir Sultan Seid, MD
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Amir Sultan Seid, MD, Martin Freeman, MD, MACG, Guru Trikudanathan, MD
University of Minnesota Medical Center, Minneapolis, MN
Introduction: Disconnected pancreatic duct syndrome (DPDS) is an underappreciated late sequalae following necrotizing pancreatitis and could manifest as recurrent pancreatic fluid collection (PFC). Double pigtailed stents (DPS) are often left indefinitely across the cystenterostomy tract to prevent PFC in the setting of DPDS. While predominantly considered safe, we hereby describe a case of erosion of a cystgastrostomy stent into the mid bile duct after four years.
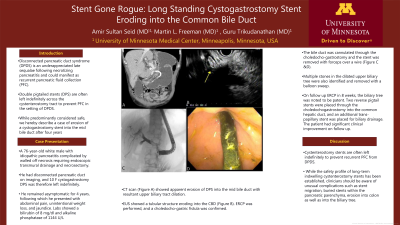
Case Description/Methods: 76-year-old white male with idiopathic pancreatitis complicated by walled off necrosis requiring endoscopic transmural drainage and necrosectomy. He had disconnected pancreatic duct on imaging, and 10 F cystgastrostomy DPS was therefore left indefinitely. He remained asymptomatic for 4 years, following which he presented with abdominal pain, unintentional weight loss, and jaundice. Labs showed a bilirubin of 8 mg/dl and alkaline phosphatase of 1144 U/L. CT scan (Figure A) showed apparent erosion of DPS into the mid bile duct with resultant upper biliary tract dilation. EUS showed a tubular structure eroding into the CBD (Figure B). ERCP was performed, and a choledocho-gastric fistula was confirmed. The bile duct was cannulated through the choledochogastrostomy and the stent was removed with forceps over a wire (Figure C &D). Multiple stones in the dilated upper biliary tree were also identified and removed with a balloon sweep. On follow up ERCP in 8 weeks, the biliary tree was noted to be patent. Two reverse pigtail stents were placed through the choledochogastrostomy into the common hepatic duct, and an additional transpapillary stent was placed for biliary drainage. The patient had significant clinical improvement on follow up.
Discussion: Cystenterostomy stents are often left indefinitely to prevent recurrent PFC from DPDS. While the safety profile of long term indwelling cystenterostomy stents has been established, clinicians should be aware of unusual complications such as stent migration, buried stents within the pancreatic parenchyma, erosion into colon as well as into the biliary tree.

Disclosures:
Amir Sultan Seid, MD, Martin Freeman, MD, MACG, Guru Trikudanathan, MD. P1483 - Stent Gone Rogue - Long Standing Cystgastrostomy Stent Eroding into the Common Bile Duct, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Minnesota Medical Center, Minneapolis, MN
Introduction: Disconnected pancreatic duct syndrome (DPDS) is an underappreciated late sequalae following necrotizing pancreatitis and could manifest as recurrent pancreatic fluid collection (PFC). Double pigtailed stents (DPS) are often left indefinitely across the cystenterostomy tract to prevent PFC in the setting of DPDS. While predominantly considered safe, we hereby describe a case of erosion of a cystgastrostomy stent into the mid bile duct after four years.
Case Description/Methods: 76-year-old white male with idiopathic pancreatitis complicated by walled off necrosis requiring endoscopic transmural drainage and necrosectomy. He had disconnected pancreatic duct on imaging, and 10 F cystgastrostomy DPS was therefore left indefinitely. He remained asymptomatic for 4 years, following which he presented with abdominal pain, unintentional weight loss, and jaundice. Labs showed a bilirubin of 8 mg/dl and alkaline phosphatase of 1144 U/L. CT scan (Figure A) showed apparent erosion of DPS into the mid bile duct with resultant upper biliary tract dilation. EUS showed a tubular structure eroding into the CBD (Figure B). ERCP was performed, and a choledocho-gastric fistula was confirmed. The bile duct was cannulated through the choledochogastrostomy and the stent was removed with forceps over a wire (Figure C &D). Multiple stones in the dilated upper biliary tree were also identified and removed with a balloon sweep. On follow up ERCP in 8 weeks, the biliary tree was noted to be patent. Two reverse pigtail stents were placed through the choledochogastrostomy into the common hepatic duct, and an additional transpapillary stent was placed for biliary drainage. The patient had significant clinical improvement on follow up.
Discussion: Cystenterostomy stents are often left indefinitely to prevent recurrent PFC from DPDS. While the safety profile of long term indwelling cystenterostomy stents has been established, clinicians should be aware of unusual complications such as stent migration, buried stents within the pancreatic parenchyma, erosion into colon as well as into the biliary tree.

Figure: Figure 1 A: CT scan coronal section showing erosion of stent originating from the stomach into the bile duct B- EUS - Echogenic tubular material in the bile duct C- ERCP - Cholangiogram via fistula tract with the stent in-situ D: Endoscopic view of the stent it the stomach cavity
Disclosures:
Amir Sultan Seid indicated no relevant financial relationships.
Martin Freeman indicated no relevant financial relationships.
Guru Trikudanathan: Boston Scientific Coporation – Consultant.
Amir Sultan Seid, MD, Martin Freeman, MD, MACG, Guru Trikudanathan, MD. P1483 - Stent Gone Rogue - Long Standing Cystgastrostomy Stent Eroding into the Common Bile Duct, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
