Monday Poster Session
Category: Biliary/Pancreas
P1517 - An Elusive Cholangiocarcinoma Mimic: Primary Biliary Tuberculosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kevin Khoury, MD
University of Chicago, NorthShore University Health Systems
Oak Brook, IL
Presenting Author(s)
Award: Presidential Poster Award
Kevin Khoury, MD1, Mitchelle Zolotarevsky, MD2, Frances Puello, MD3, Edward C. Villa, MD4
1University of Chicago, NorthShore University Health Systems, Oak Brook, IL; 2University of Chicago, NorthShore Internal Medicine, Evanston, IL; 3University of Chicago/Northshore, Evanston, IL; 4University of Chicago, NorthShore Health Systems, Evanston, IL
Introduction: Extrapulmonary tuberculosis of the biliary tract is an elusive diagnosis, difficult to diagnosis given nonspecific symptoms and imaging studies. Historically, the diagnosis has been reliant on pathology, when technically feasible, but often requires surgical biopsy. We report here a case of primary biliary tuberculosis diagnosed with the assistance of cholangioscopic biopsies and endoscopic ultrasound (EUS) fine needle biopsies.
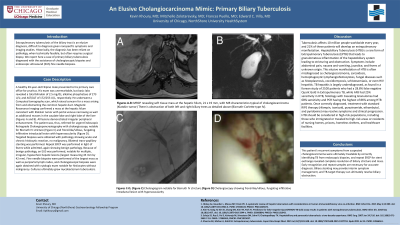
Case Description/Methods: A healthy 49-year-old Filipino male presented to his primary care office for pruritus. His exam was unremarkable, but basic labs revealed a total bilirubin of 2.5 mg/dL; alkaline phosphatase of 273 U/L; and AST/ALT of 172/253 U/L, respectively. He underwent a Computed tomography scan, which raised concern for a mass arising from and obstructing the common hepatic duct. Magnetic Resonance Imaging confirmed a mass at the hepatic hilum consistent with Klatskin tumor with portal venous narrowing as well as additional masses in the caudate lobe and right lobe of the liver (Figures A and B). All lesions demonstrated irregular peripheral enhancement. The patient was, thus, referred for urgent Endoscopic Retrograde Cholangiopancreatography with cholangioscopy, notable for Bismuth IV stricture (Figure C) and frond-like/villous, fungating infiltrative intraductal lesion with hypervascularity (Figure D). Targeted biopsies were obtained with pathology showed acute and chronic histiocytic reaction, no malignancy. Bilateral transpapillary stenting was performed. Repeat ERCP was performed in light of fevers while admitted, again showing benign pathology. Because of benign pathology, an EUS was performed, notable for multiple, irregular, hypoechoic hepatic lesions (largest measuring 43 mm by 42 mm). Fine needle biopsies were performed of the largest mass as well as periportal lymph nodes, and cholangioscopic biopsies were again obtained with cytologic exam notable for histiocytes without malignancy. Cultures ultimately grew mycobacterium tuberculosis.
Discussion: Hepatobiliary tuberculosis can present as biliary stricture(s) and mass(es), mimicking cholangiocarcinoma. Biliary tuberculosis is a particularly rare presentation of tuberculosis and is exceptionally rare as isolated extrapulmonary tuberculosis. Biliary tuberculosis is often reported as a diagnostic dilemma, as the diagnosis relies on tissue examination, and even the most advanced imaging modalities can lead to an incorrect diagnosis, as depicted in our case.

Disclosures:
Kevin Khoury, MD1, Mitchelle Zolotarevsky, MD2, Frances Puello, MD3, Edward C. Villa, MD4. P1517 - An Elusive Cholangiocarcinoma Mimic: Primary Biliary Tuberculosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Kevin Khoury, MD1, Mitchelle Zolotarevsky, MD2, Frances Puello, MD3, Edward C. Villa, MD4
1University of Chicago, NorthShore University Health Systems, Oak Brook, IL; 2University of Chicago, NorthShore Internal Medicine, Evanston, IL; 3University of Chicago/Northshore, Evanston, IL; 4University of Chicago, NorthShore Health Systems, Evanston, IL
Introduction: Extrapulmonary tuberculosis of the biliary tract is an elusive diagnosis, difficult to diagnosis given nonspecific symptoms and imaging studies. Historically, the diagnosis has been reliant on pathology, when technically feasible, but often requires surgical biopsy. We report here a case of primary biliary tuberculosis diagnosed with the assistance of cholangioscopic biopsies and endoscopic ultrasound (EUS) fine needle biopsies.
Case Description/Methods: A healthy 49-year-old Filipino male presented to his primary care office for pruritus. His exam was unremarkable, but basic labs revealed a total bilirubin of 2.5 mg/dL; alkaline phosphatase of 273 U/L; and AST/ALT of 172/253 U/L, respectively. He underwent a Computed tomography scan, which raised concern for a mass arising from and obstructing the common hepatic duct. Magnetic Resonance Imaging confirmed a mass at the hepatic hilum consistent with Klatskin tumor with portal venous narrowing as well as additional masses in the caudate lobe and right lobe of the liver (Figures A and B). All lesions demonstrated irregular peripheral enhancement. The patient was, thus, referred for urgent Endoscopic Retrograde Cholangiopancreatography with cholangioscopy, notable for Bismuth IV stricture (Figure C) and frond-like/villous, fungating infiltrative intraductal lesion with hypervascularity (Figure D). Targeted biopsies were obtained with pathology showed acute and chronic histiocytic reaction, no malignancy. Bilateral transpapillary stenting was performed. Repeat ERCP was performed in light of fevers while admitted, again showing benign pathology. Because of benign pathology, an EUS was performed, notable for multiple, irregular, hypoechoic hepatic lesions (largest measuring 43 mm by 42 mm). Fine needle biopsies were performed of the largest mass as well as periportal lymph nodes, and cholangioscopic biopsies were again obtained with cytologic exam notable for histiocytes without malignancy. Cultures ultimately grew mycobacterium tuberculosis.
Discussion: Hepatobiliary tuberculosis can present as biliary stricture(s) and mass(es), mimicking cholangiocarcinoma. Biliary tuberculosis is a particularly rare presentation of tuberculosis and is exceptionally rare as isolated extrapulmonary tuberculosis. Biliary tuberculosis is often reported as a diagnostic dilemma, as the diagnosis relies on tissue examination, and even the most advanced imaging modalities can lead to an incorrect diagnosis, as depicted in our case.

Figure: A and B) MRCP revealing mass at the hepatic hilum consistent with Klatskin tumor with portal venous narrowing as well as additional mass lesions noted in the caudate lobe and right lobe of the liver C) Cholangiogram notable for Bismuth IV stricture (Figure C) Cholangioscopy showing frond-like/villous, fungating infiltrative intraductal lesion with hypervascularity
Disclosures:
Kevin Khoury indicated no relevant financial relationships.
Mitchelle Zolotarevsky indicated no relevant financial relationships.
Frances Puello indicated no relevant financial relationships.
Edward Villa: Interscope – Consultant. Medtronic plc – Consultant. Noah Medical Inc – Consultant. Olympus Corp – Consultant.
Kevin Khoury, MD1, Mitchelle Zolotarevsky, MD2, Frances Puello, MD3, Edward C. Villa, MD4. P1517 - An Elusive Cholangiocarcinoma Mimic: Primary Biliary Tuberculosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


