Monday Poster Session
Category: Biliary/Pancreas
P1518 - The Case of a Disrupted Pancreatic Duct with Necrotic Fluid Collection, Treated with Endoscopic Management
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Amir Aghaabdollah, DO
HCA Healthcare/USF Morsani College of Medicine: HCA Florida Largo Hospital
Largo, FL
Presenting Author(s)
Amir Aghaabdollah, DO1, Kelly Volland, DO1, Anabel Rodriguez Loya, DO2, Meir Mizrahi, MD2
1HCA Healthcare/USF Morsani College of Medicine: HCA Florida Largo Hospital, Largo, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: There have been continued changes to the treatment approach for pancreatic duct trauma, with there being a combination of surgical, endoscopic, and interventional approaches. This case involves endoscopic management of pancreatic duct disruption, after a motor vehicle accident.
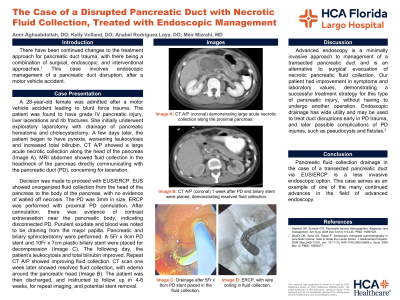
Case Description/Methods: A 28-year-old female was admitted after a motor vehicle accident leading to blunt force trauma. The patient was found to have grade IV pancreatic injury, liver lacerations and rib fractures. She initially underwent exploratory laparotomy with drainage of pancreatic hematoma and cholecystectomy. A few days later, the patient began to have pyrexia, worsening leukocytosis and increased total bilirubin. CT A/P showed a large acute necrotic collection along the head of the pancreas (a). MRI abdomen showed fluid collection in the head/neck of the pancreas directly communicating with the PD, concerning for laceration. Patient was then taken for EUS/ERCP. EUS showed unorganized fluid collection from the head of the pancreas to the body of the pancreas, with no evidence of walled off necrosis. The PD was 3mm in size. ERCP was performed with proximal PD cannulation. After cannulation, there was evidence of contrast extravasation near the pancreatic body, indicating disconnected PD. Purulent exudate and blood was noted to be draining from the major papilla. Pancreatic and biliary sphincterotomy were performed. A 5Fr x 8cm PD stent and 10Fr x 7cm plastic biliary stent were placed for decompression (c). The following day, the patient’s leukocytosis and total bilirubin improved. Repeat CT A/P showed improving fluid collection. CT scan 1 week later showed resolved fluid collection, with edema around the pancreatic head (b). The patient was then discharged, and instructed to follow up in 4-6 weeks, for repeat imaging, and potential stent removal.
Discussion: Advanced endoscopy is a minimally invasive approach to management of a transected PD and is an alternative to surgical evacuation of necrotic pancreatic fluid collection. Our patient had improvement in symptoms and laboratory values, demonstrating a successful treatment strategy for this type of pancreatic injury, without having to undergo another operation. Endoscopic drainage has wide utility and may be used to treat duct disruptions early in PD trauma, and later possible complications of PD injuries. This case serves as an example of one of the many continued advances in the field of advanced endoscopy.

Disclosures:
Amir Aghaabdollah, DO1, Kelly Volland, DO1, Anabel Rodriguez Loya, DO2, Meir Mizrahi, MD2. P1518 - The Case of a Disrupted Pancreatic Duct with Necrotic Fluid Collection, Treated with Endoscopic Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA Healthcare/USF Morsani College of Medicine: HCA Florida Largo Hospital, Largo, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: There have been continued changes to the treatment approach for pancreatic duct trauma, with there being a combination of surgical, endoscopic, and interventional approaches. This case involves endoscopic management of pancreatic duct disruption, after a motor vehicle accident.
Case Description/Methods: A 28-year-old female was admitted after a motor vehicle accident leading to blunt force trauma. The patient was found to have grade IV pancreatic injury, liver lacerations and rib fractures. She initially underwent exploratory laparotomy with drainage of pancreatic hematoma and cholecystectomy. A few days later, the patient began to have pyrexia, worsening leukocytosis and increased total bilirubin. CT A/P showed a large acute necrotic collection along the head of the pancreas (a). MRI abdomen showed fluid collection in the head/neck of the pancreas directly communicating with the PD, concerning for laceration. Patient was then taken for EUS/ERCP. EUS showed unorganized fluid collection from the head of the pancreas to the body of the pancreas, with no evidence of walled off necrosis. The PD was 3mm in size. ERCP was performed with proximal PD cannulation. After cannulation, there was evidence of contrast extravasation near the pancreatic body, indicating disconnected PD. Purulent exudate and blood was noted to be draining from the major papilla. Pancreatic and biliary sphincterotomy were performed. A 5Fr x 8cm PD stent and 10Fr x 7cm plastic biliary stent were placed for decompression (c). The following day, the patient’s leukocytosis and total bilirubin improved. Repeat CT A/P showed improving fluid collection. CT scan 1 week later showed resolved fluid collection, with edema around the pancreatic head (b). The patient was then discharged, and instructed to follow up in 4-6 weeks, for repeat imaging, and potential stent removal.
Discussion: Advanced endoscopy is a minimally invasive approach to management of a transected PD and is an alternative to surgical evacuation of necrotic pancreatic fluid collection. Our patient had improvement in symptoms and laboratory values, demonstrating a successful treatment strategy for this type of pancreatic injury, without having to undergo another operation. Endoscopic drainage has wide utility and may be used to treat duct disruptions early in PD trauma, and later possible complications of PD injuries. This case serves as an example of one of the many continued advances in the field of advanced endoscopy.

Figure: Image a: CT A/P (coronal) demonstrating large acute necrotic collection along the proximal pancreas.
Image b: CT A/P (coronal) 1 week after PD and biliary stent were placed, demonstrating resolved fluid collection.
Image c: Drainage after 5Fr x 8cm PD stent placed in the fluid collection.
Image d: ERCP, with wire coiling in fluid collection.
Image b: CT A/P (coronal) 1 week after PD and biliary stent were placed, demonstrating resolved fluid collection.
Image c: Drainage after 5Fr x 8cm PD stent placed in the fluid collection.
Image d: ERCP, with wire coiling in fluid collection.
Disclosures:
Amir Aghaabdollah indicated no relevant financial relationships.
Kelly Volland indicated no relevant financial relationships.
Anabel Rodriguez Loya indicated no relevant financial relationships.
Meir Mizrahi indicated no relevant financial relationships.
Amir Aghaabdollah, DO1, Kelly Volland, DO1, Anabel Rodriguez Loya, DO2, Meir Mizrahi, MD2. P1518 - The Case of a Disrupted Pancreatic Duct with Necrotic Fluid Collection, Treated with Endoscopic Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
