Monday Poster Session
Category: Biliary/Pancreas
P1524 - Unveiling the Link: Hypertriglyceridemia Induced Acute Pancreatitis in a Young Female on Oral Contraceptives - A Case Report
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KT
Kelsey Theriault, DO
Florida State University
Cape Coral, FL
Presenting Author(s)
Gautam Maddineni, MD1, Katarzyna Karpinska Leydier, MD1, Silpa Choday, MD2, Kelsey Theriault, DO1, Abraham Bell, DO1, Augustine Salami, MD1, Dustin Begosh- Mayne, MD1
1Florida State University, Cape Coral, FL; 2Creighton University, Phoenix, AZ
Introduction: Acute pancreatitis is a common gastrointestinal presentation in the emergency department and can lead to significant morbidity and mortality. Hypertriglyceridemia is the third most common cause of acute pancreatitis, accounting for approximately 7% of cases. Oral contraceptive pills (OCPs) cause secondary hypertriglyceridemia because of estrogen, which can lead to elevated triglyceride levels and potentially contribute to the development of acute pancreatitis.
Case Description/Methods: A 24-year-old female with a history of cystic acne on spironolactone and Loryna (drospirenone and ethinyl estradiol tablets) presented to the Emergency Department with severe left flank pain rated 9/10. Nausea and non-bloody, non-bilious vomiting were also reported. Laboratory tests revealed an elevated white blood cell count, high anion gap, elevated lipase, and significantly high cholesterol (650mg/dL) and triglyceride levels ( >1575mg/dL, upper limit of the test). Imaging studies confirmed inflammation in the pancreatic body and tail with fluid accumulation in the abdomen and pelvis.
Management involved NPO status, an insulin drip, discontinuation of Loryna and spironolactone, and initiating Gemfibrozil and Omega 3 therapy. Triglyceride levels decreased to 315mg/dL over six days of treatment. Genetic testing ruled out familial hypertriglyceridemia syndromes and polygenic risk factors associated with hypertriglyceridemia.
Discussion: This case report highlights the association between acute pancreatitis and Loryna. Estrogen in oral contraceptives can cause secondary hypertriglyceridemia by reducing hepatic triglyceride lipase and lipoprotein lipase activity. Previous studies have linked estrogen-containing contraceptives to acute pancreatitis. Regular triglyceride monitoring in oral contraceptive users, especially those with a history of hyperlipidemia, may help prevent complications. Discontinuation of oral contraceptives often normalizes triglyceride levels, supporting their role as the likely cause.
In conclusion, this case report emphasizes the association between oral contraceptive use, hypertriglyceridemia, and acute pancreatitis. Prescribers should exercise caution and consider the potential risks of estrogen-based medications. Regular triglyceride monitoring and exploration of alternative contraceptive options may benefit high-risk patients. Further research is needed to assess the value of routine triglyceride monitoring in oral contraceptive users.

Disclosures:
Gautam Maddineni, MD1, Katarzyna Karpinska Leydier, MD1, Silpa Choday, MD2, Kelsey Theriault, DO1, Abraham Bell, DO1, Augustine Salami, MD1, Dustin Begosh- Mayne, MD1. P1524 - Unveiling the Link: Hypertriglyceridemia Induced Acute Pancreatitis in a Young Female on Oral Contraceptives - A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Florida State University, Cape Coral, FL; 2Creighton University, Phoenix, AZ
Introduction: Acute pancreatitis is a common gastrointestinal presentation in the emergency department and can lead to significant morbidity and mortality. Hypertriglyceridemia is the third most common cause of acute pancreatitis, accounting for approximately 7% of cases. Oral contraceptive pills (OCPs) cause secondary hypertriglyceridemia because of estrogen, which can lead to elevated triglyceride levels and potentially contribute to the development of acute pancreatitis.
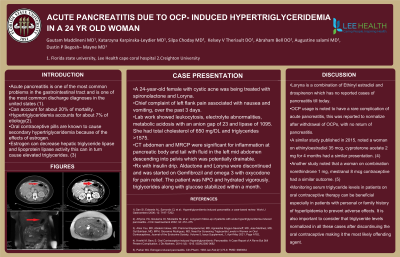
Case Description/Methods: A 24-year-old female with a history of cystic acne on spironolactone and Loryna (drospirenone and ethinyl estradiol tablets) presented to the Emergency Department with severe left flank pain rated 9/10. Nausea and non-bloody, non-bilious vomiting were also reported. Laboratory tests revealed an elevated white blood cell count, high anion gap, elevated lipase, and significantly high cholesterol (650mg/dL) and triglyceride levels ( >1575mg/dL, upper limit of the test). Imaging studies confirmed inflammation in the pancreatic body and tail with fluid accumulation in the abdomen and pelvis.
Management involved NPO status, an insulin drip, discontinuation of Loryna and spironolactone, and initiating Gemfibrozil and Omega 3 therapy. Triglyceride levels decreased to 315mg/dL over six days of treatment. Genetic testing ruled out familial hypertriglyceridemia syndromes and polygenic risk factors associated with hypertriglyceridemia.
Discussion: This case report highlights the association between acute pancreatitis and Loryna. Estrogen in oral contraceptives can cause secondary hypertriglyceridemia by reducing hepatic triglyceride lipase and lipoprotein lipase activity. Previous studies have linked estrogen-containing contraceptives to acute pancreatitis. Regular triglyceride monitoring in oral contraceptive users, especially those with a history of hyperlipidemia, may help prevent complications. Discontinuation of oral contraceptives often normalizes triglyceride levels, supporting their role as the likely cause.
In conclusion, this case report emphasizes the association between oral contraceptive use, hypertriglyceridemia, and acute pancreatitis. Prescribers should exercise caution and consider the potential risks of estrogen-based medications. Regular triglyceride monitoring and exploration of alternative contraceptive options may benefit high-risk patients. Further research is needed to assess the value of routine triglyceride monitoring in oral contraceptive users.

Figure: CT abdomen findings
Disclosures:
Gautam Maddineni indicated no relevant financial relationships.
Katarzyna Karpinska Leydier indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Kelsey Theriault indicated no relevant financial relationships.
Abraham Bell indicated no relevant financial relationships.
Augustine Salami indicated no relevant financial relationships.
Dustin Begosh- Mayne indicated no relevant financial relationships.
Gautam Maddineni, MD1, Katarzyna Karpinska Leydier, MD1, Silpa Choday, MD2, Kelsey Theriault, DO1, Abraham Bell, DO1, Augustine Salami, MD1, Dustin Begosh- Mayne, MD1. P1524 - Unveiling the Link: Hypertriglyceridemia Induced Acute Pancreatitis in a Young Female on Oral Contraceptives - A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
