Monday Poster Session
Category: Biliary/Pancreas
P1527 - Necrotizing Pancreatitis After Bland Embolization of a Large Hepatic Hemangioma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AK
Ayesha Khan, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Ayesha Khan, DO, Julia Hawes, BS, Julia Zhang, MD, Karen Szauter, MD, Sreeram Parupudi, MD
University of Texas Medical Branch, Galveston, TX
Introduction: Liver embolization is a common procedure for management of malignant and nonmalignant liver lesions. Embolization can be performed through a bland technique using only embolic material or by chemotherapy agents. Infrequent complications seen post liver embolization are pulmonary thromboembolism, hepatic infarct, liver abscess, liver failure, ischemic biliary strictures, and less frequently pancreatic damage (incidence of 1.7%). We describe a case of necrotizing pancreatitis after bland embolization of a large hepatic hemangioma.
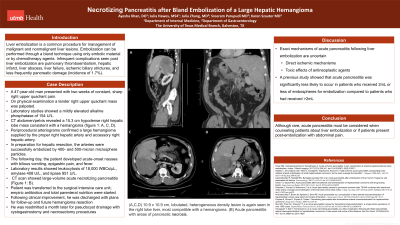
Case Description/Methods: A 47-year-old man presented with two weeks of constant, sharp right upper without associated symptoms. On physical examination a tender right upper quadrant mass was palpated. Admission laboratory studies showed a mildly elevated alkaline phosphatase of 154 U/L. The remaining liver profile, complete blood count, and basic metabolic panel were normal. Abdominal computed tomography (CT) scan revealed a 15.3 cm hypodense right hepatic lobe mass consistent with a hemangioma. Periprocedural arteriograms confirmed a large hemangioma supplied by the proper right hepatic artery and accessory right hepatic artery. In preparation for hepatic resection, the arteries were successfully embolized by 400- and 500-micron microsphere particles. The following day, the patient developed acute-onset nausea with bilious vomiting, epigastric pain, and fever. Laboratory results showed a leukocytosis of 18,000 WBCs/µL, amylase 408 U/L, and lipase 951 U/L; CT scan revealed a large-volume acute necrotizing pancreatitis. He was transferred to the surgical intensive care unit; empiric antibiotics and total parenteral nutrition were started. Following clinical improvement, he was discharged with plans for follow-up and future hemangioma resection. He was readmitted a month later for pseudocyst drainage with cystogastrostomy and necrosectomy procedures.
Discussion: The exact mechanisms of acute pancreatitis following liver embolization is uncertain although direct ischemic mechanisms and toxic effects of antineoplastic agents are thought to play a role. A previous study showed that acute pancreatitis was significantly less likely to occur in patients who received 2mL or less of embospheres for embolization compared to patients who had received >2mL. Although rare, acute pancreatitis must be considered when counseling patients about liver embolization or if patients present post-embolization abdominal pain.

Disclosures:
Ayesha Khan, DO, Julia Hawes, BS, Julia Zhang, MD, Karen Szauter, MD, Sreeram Parupudi, MD. P1527 - Necrotizing Pancreatitis After Bland Embolization of a Large Hepatic Hemangioma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Texas Medical Branch, Galveston, TX
Introduction: Liver embolization is a common procedure for management of malignant and nonmalignant liver lesions. Embolization can be performed through a bland technique using only embolic material or by chemotherapy agents. Infrequent complications seen post liver embolization are pulmonary thromboembolism, hepatic infarct, liver abscess, liver failure, ischemic biliary strictures, and less frequently pancreatic damage (incidence of 1.7%). We describe a case of necrotizing pancreatitis after bland embolization of a large hepatic hemangioma.
Case Description/Methods: A 47-year-old man presented with two weeks of constant, sharp right upper without associated symptoms. On physical examination a tender right upper quadrant mass was palpated. Admission laboratory studies showed a mildly elevated alkaline phosphatase of 154 U/L. The remaining liver profile, complete blood count, and basic metabolic panel were normal. Abdominal computed tomography (CT) scan revealed a 15.3 cm hypodense right hepatic lobe mass consistent with a hemangioma. Periprocedural arteriograms confirmed a large hemangioma supplied by the proper right hepatic artery and accessory right hepatic artery. In preparation for hepatic resection, the arteries were successfully embolized by 400- and 500-micron microsphere particles. The following day, the patient developed acute-onset nausea with bilious vomiting, epigastric pain, and fever. Laboratory results showed a leukocytosis of 18,000 WBCs/µL, amylase 408 U/L, and lipase 951 U/L; CT scan revealed a large-volume acute necrotizing pancreatitis. He was transferred to the surgical intensive care unit; empiric antibiotics and total parenteral nutrition were started. Following clinical improvement, he was discharged with plans for follow-up and future hemangioma resection. He was readmitted a month later for pseudocyst drainage with cystogastrostomy and necrosectomy procedures.
Discussion: The exact mechanisms of acute pancreatitis following liver embolization is uncertain although direct ischemic mechanisms and toxic effects of antineoplastic agents are thought to play a role. A previous study showed that acute pancreatitis was significantly less likely to occur in patients who received 2mL or less of embospheres for embolization compared to patients who had received >2mL. Although rare, acute pancreatitis must be considered when counseling patients about liver embolization or if patients present post-embolization abdominal pain.

Figure: (A,C,D) 10.9 x 10.9 cm, lobulated, heterogeneous density lesion is again seen in the right lobe liver, most compatible with a hemangioma. (B) Acute pancreatitis with areas of pancreatic necrosis.
Disclosures:
Ayesha Khan indicated no relevant financial relationships.
Julia Hawes indicated no relevant financial relationships.
Julia Zhang indicated no relevant financial relationships.
Karen Szauter indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Ayesha Khan, DO, Julia Hawes, BS, Julia Zhang, MD, Karen Szauter, MD, Sreeram Parupudi, MD. P1527 - Necrotizing Pancreatitis After Bland Embolization of a Large Hepatic Hemangioma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
